Four Key Elements of Esthetic Dentistry and the Importance of the Prototype
Every time the interdisciplinary team embarks on the complex process of reconstructing a patient with either a debilitated or terminal dentition, the outcome depends on the amount of detail in the communication. To ensure a more successful outcome, here are four key elements of esthetic dentistry that must be specified when transferring esthetic and functional parameters to the ceramist.
Transitioning a patient with either terminal dentition or a fully edentulous condition typically involves using a set of provisional restorations. These typically range from:
- A conversion of pre-existing dentures.
- A conversion of a set of immediate dentures.
- A new CAD/CAM-generated provisional restoration.
Regardless of which is used, their fabrication entails some “guess-estimation” to attain ballpark esthetic and functional parameters during the initial provisionalization stage.

Because of the vast number of prosthetic design details (both esthetic and functional) that need to be considered during the fabrication of the definitive prosthesis, using a prototype (blueprint template) is the ultimate means of communication between the clinician and the patient and between the clinician and the technician.

The 4 Key Elements of Esthetic Dentistry
By breaking things up into the four essential key elements of esthetic dentistry, the team has a much better chance to communicate successfully and therefore calibrate everyone’s expectations through the following parameters:
- Color
- Contour
- Arrangement
- Position and Functional Parameters
Color: The Shade of Their New Smile
Shade selection must be thoroughly discussed with patients, leaving no room for misunderstanding. Agreeing on the desired shade can be tricky. In this era of the so-called “Hollywood smile,” many patients are looking for a white tooth color that may not be our preferred selection as clinicians, since we know that such extremely bright shades are unnatural and typically produce a “fake” look. We need to educate the patient before they make their final decision, but in the end, while we may express our informed opinion, it is the patient’s choice.
The last thing we want to occur during the insertion appointment of a sophisticated CAD/CAM-generated, implant-supported reconstruction is for our patients to be surprised and unhappy about the shade of their new smile. This is especially true when patients feel the teeth are not white enough, since there is no simple correction to address this concern — it usually entails redoing a sizable portion of the work, generating enormous frustration for everyone involved, starting with the patient.
There is typically so much expectation built around the insertion appointment that not giving patients the “smile of their dreams” lets them down. However, that same expectation is built up on our end; the treating team is usually also excited to insert the ceramic reconstruction, as it represents the culmination of an elaborate treatment that should be life-changing for our patient and, therefore, extremely rewarding for us.
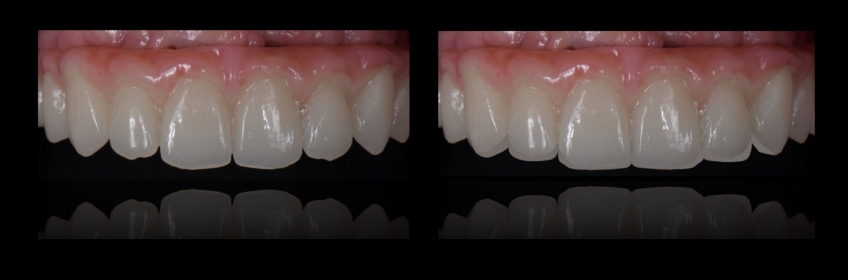
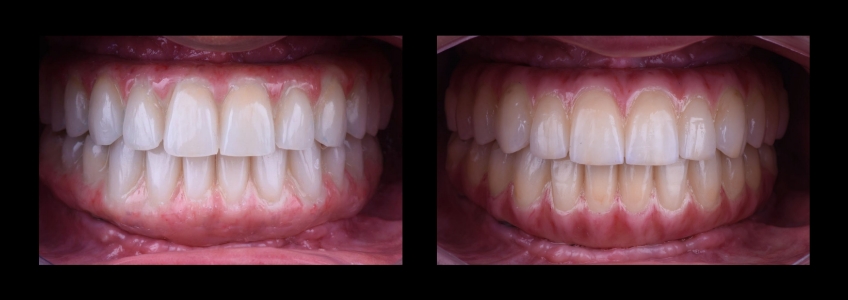
It is also important to point out that when doing a prototype try-in, we deal with a material different from the definitive prosthesis. The prototype will typically be made of PMMA, while the definitive reconstruction will be made of zirconia. And even though the technician will use the same shade from our shade guide, some important optical properties will be perceived differently when comparing both materials. Properties such as translucency, opalescence, and fluorescence will vary, and these variances should also be thoroughly communicated to the patient so that they can appreciate the nuances between both materials.

Contour: Choosing a Square, Ovoid or Triangular Shape
This refers to the shape of the teeth. While there are wide-ranging shape libraries, we try to simplify the process by keeping things in the realm of three generic shapes: square, ovoid, and triangular.

This parameter needs to be conveyed to the patients so we can get as much input as possible. As part of the consultative process, it can be of significant help to get photographs of the patient in their younger years and/or photographs of family members such as siblings or children, as there are definitive genetic patterns that we could easily gather and that will aid in our contour discussion and selection.
An important thing to note: if patients express a specific desire for triangular shapes, and we are not considering adding any pink ceramics to the definitive reconstruction, it will be next to impossible to attain natural long interproximal papillae, which are typically seen between natural triangular teeth. This is because usually, for these shaped teeth, there is a shorter contact area between teeth than seen with ovoid- or square-shaped teeth, and such contact area is situated more towards the incisal edge. Also, there is an accentuated scallop in both the soft and hard tissues, and, lastly, there is a well-defined interproximal peak of bone supporting such papillae.
When teeth are lost, there is an inevitable remodeling process of such interproximal peaks of bone, to the point where it becomes impossible to support long natural soft tissues interproximally. We must manage this soft tissue deficiency by leaving a black triangle (which patients often dislike) or broadening the contact area, creating a more squarish-looking tooth.
It should be noted, however, that in everyday situations where we are dealing with vertical ridge defects, incorporating pink ceramics to compensate for the vertical ridge defect becomes important in creating teeth with pleasing proportions. In these cases, choosing triangular-shaped teeth and incorporating interproximal pink ceramics is definitely doable if the patient desires this.
So, once again, it’s essential to discuss these biologic limitations regarding tooth contour to preemptively manage patients’ expectations.

Arrangement: Keeping It Natural
Arrangement refers to the composition of the teeth — in other words, how one tooth relates to the adjacent teeth. A more natural arrangement is one where we can see subtle imperfections or asymmetry across the smile. Teeth move due to age, so incorporating slight rotations can significantly improve the smile’s natural look.
As we discussed earlier, with color and patients wanting a perfectly white shade, a perfectly aligned and symmetrical arrangement in an adult patient usually indicates a “not so natural” smile. We should embrace the opportunity to educate our patients regarding our perception of tooth arrangement, and a common “imperfection,” which is usually age-related, is dental wear. This will typically manifest as decreased interincisal angles among the anterior maxillary teeth. An arrangement that factors in this reality will appear more natural.
Position Parameters: The Fundamentals
When it comes to position, we need to break it down into four additional fundamental parameters:
1. Midline
Ideally, consider the patient’s facial midline, a line that dissects the patient’s face into two halves, as a reference. The “cupid’s bow” in the upper lip is a closer reference as we zoom into the smile and determine the position and orientation of the prosthetic dental midline in our implant-supported reconstruction.
Remember that most patients are not facially symmetric, making it tricky to “nail down” the midline. The key is that our prosthetic midline should be parallel to a line that dissects the patient’s face and perpendicular to a horizontal line depicting the horizon.
2. Incisal Plane
This is usually called the smile line, which results when we connect the incisal edges of the six anterior teeth. This incisal plane should follow the lower lip, be parallel to the horizon, and be perpendicular to the midline.
The incisal plane needs to be evaluated in both a frontal and sagittal perspective, as its position is closely interdependent with the patient’s lips.
From a frontal perspective, we want to ensure that there is at least minimal incisal edge display in repose so patients do not have an “edentulous look.” Depending on the patient’s age and gender, we may consider such an incisal display anywhere from 1.0 mm to 3.0 mm.
From a sagittal perspective, the anteroposterior position of the incisal edge should provide adequate and pleasing lip support. The references that we follow to attain this are both from the orthodontic world:
- Ricketts “E” plane: A line from the nose’s tip to the chin’s tip is viewed sagittally.
- Upper lip 4.0 mm behind the planeLower lip 2.0 mm behind the plane
- Andrew’s line: Antero-posterior relationship of the maxillary incisor to the forehead. We must correct the patient’s head posture to use this as a reference. And the goal is to have the facial aspect of the maxillary incisor on the same plane as the glabella.
3. Occlusal Plane
The imaginary line that dissects the cusp tips of the posterior teeth is a distal projection or continuation of the incisal plane.
It should be evaluated from a frontal perspective, intraorally, and extra-orally. To verify that the orientation of the incisal and occlusal planes is “somewhat parallel” to the horizon, there is a specific photograph you want to get.
As photographers, we tend to “compensate through the lens” by tilting our camera whenever we see an orientation discrepancy. This is a mistake, as it perpetuates discrepancies when moving forward to the fabrication of the definitive restorations. Dealing with these discrepancies and correcting the orientation of the occlusal plane should be addressed sooner rather than later.
Therefore, to accurately capture the orientation of the incisal and occlusal planes, we need to take an extraoral picture using plastic lip retractors and ask the patient to smile with an upright head posture. This allows us to remove the lips momentarily from the equation and focus our attention on assessing the orientation of the prototype’s incisal/occlusal plane relative to the horizon.
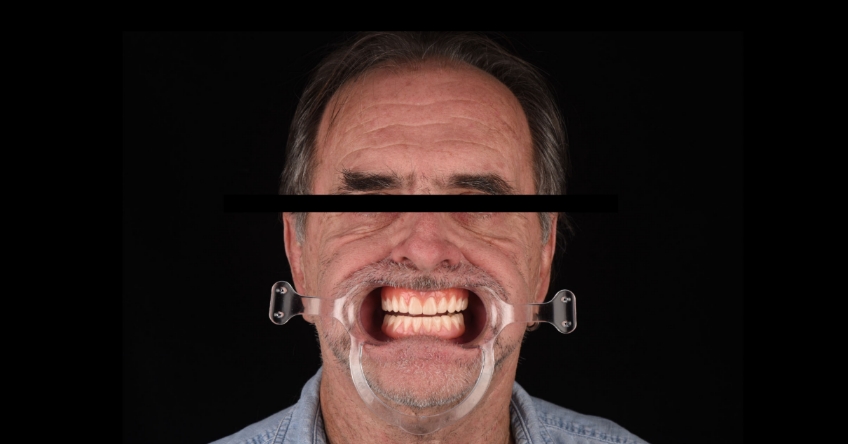
Here, we must ensure we have a nicely harmonious parallel plane. If there are occlusal cants, it is now that the treating team needs to adjust accordingly (either additive or subtractive) before sending it back to the ceramist so it can be used as a reference for the fabrication of the definitive ceramic restorations.
Seeing minor cants of the incisal/occlusal plane at this stage of the game is not uncommon, so it becomes a crucial aspect in data transferring to ensure a successful esthetic integration.
Lastly, we need to assess the transverse position of the occlusal plane as yet another fundamental aspect of our esthetic, but also functional, checklist.
4. Gingival Outline
The treating team usually strives for relative symmetry when assessing the gingival plane or outline. Traditionally, the gingival margins of the central incisors and canines are leveled, and the margins of the lateral incisors are slightly coronal to them, or at least at the same level. It usually seems unharmonious to see the gingival levels of the lateral incisors in a more apical position than the centrals and canines.

Talking about all these esthetic dentistry parameters with our patients needs to be part of an earlier discussion, but the prototype try-in should be a confirmation that every single aspect has been successfully dialed in and transferred so that the definitive ceramic outcome is 100% satisfactory for both the patient and the treating team.
Functional Parameters
The prototype try-in appointment is also critical from a functional standpoint, as it verifies that the laboratory has an accurate transfer of the occlusion and, therefore, can safely take the case to completion without the need for additional extensive occlusal adjustment.
This is particularly important since the most common materials of choice in contemporary implant-supported reconstructions have become monolithic zirconia restorations, or at least zirconia on the occlusal surfaces with a minimal cutback for overlaying ceramics in the facial aspect of the anterior teeth. Therefore, the treating team wants to minimize the occlusal adjustment needed during the insertion of the definitive prosthesis.
The occlusal scheme in full-mouth implant-supported reconstructions consists of attaining multiple simultaneous, homogeneous, evenly distributed occlusal contacts in all posterior teeth, as well as the anterior teeth.
While assessing eccentric mandibular movements, the occlusal scheme we are looking for with these patients is to provide shallow anterior guidance and a shallow canine rise to minimize the torsional stress applied to the restorative materials. (This is recommended when dealing with fixed restorations on both arches.)
Once we adjust and verify the occlusal scheme on the prototype try-in appointment, it becomes extremely easy to transfer these functional parameters to the definitive ceramic restorations and avoid extensive adjustments during the insertion appointment.
Depending on how closely we attained these parameters with the previous provisional restoration, the treating team may insert the prototype for some time so the patient can road test it and then provide feedback so we can make changes accordingly.
There will be instances when we can nail most of these parameters with the initial provisional. The prototype will only be used to communicate specific details on how we need to enhance the transverse position of the posterior teeth and provide a more pleasing buccal corridor. In this case, we can use a temporary cylinder to secure the prototype during try-in.

Once this is tried in and verified, it becomes straightforward to fabricate the definitive prosthesis.

After reviewing this systematic assessment and the four key elements of esthetic dentistry, treating clinicians can appreciate the significant advantages of using the prototype as a fundamental step of treatment and convey this information to the patient as the ultimate opportunity to verify and validate that all esthetic and functional parameters are met before moving forward to the insertion of the definitive prosthesis.

References
Vinha, P. P., Thuler, E. R., & de Mello-Filho, F. V. (2020). Effects of surgically assisted rapid maxillary expansion on the modification of the pharynx and hard palate and on obstructive sleep apnea, and their correlations.Journal of Cranio-Maxillofacial Surgery,48(4), 339-348.
Ricketts, R. M. (1968). Esthetics, environment, and the law of lip relation.American journal of orthodontics,54(4), 272-289.
Andrews, W. A. (2008). AP relationship of the maxillary central incisors to the forehead in adult white females.The Angle Orthodontist,78(4), 662-669.
Thuler, E., Rabelo, F. A., Yui, M., Tominaga, Q., dos Santos Jr, V., & Arap, S. S. (2021). Correlation between the transverse dimension of the maxilla, upper airway obstructive site, and OSA severity.Journal of Clinical Sleep Medicine,17(7), 1465-1473.
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Ricardo Mitrani
Date: October 13, 2022
Featured Digest articles
Insights and advice from Spear Faculty and industry experts