Terminal Dentition: Where Do We Draw the Line?
Have you ever heard a patient say they have terminal dentition? Probably not. Terminal dentition is a dental term made up by clinicians who ultimately decide the fate of a patient’s remaining teeth based on their personal parameters, clinical experience, and beliefs. It can be a risky decision, too, since the clinician must walk a fine line between being negligent and over-treating a patient’s condition.
The fundamental aspects of concluding terminal dentition should be influenced by the patient’s systemic condition, financial situation, and the patient’s chief complaint.
So, is it possible for clinicians to decide whether to extract or preserve a patient’s teeth based on clinical and radiographic diagnostic evaluation?
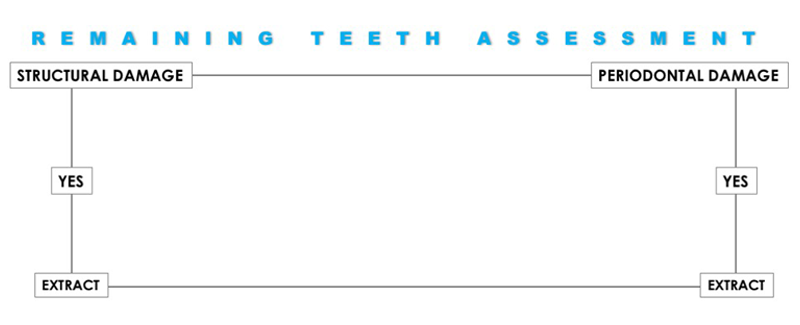
Decision Tree
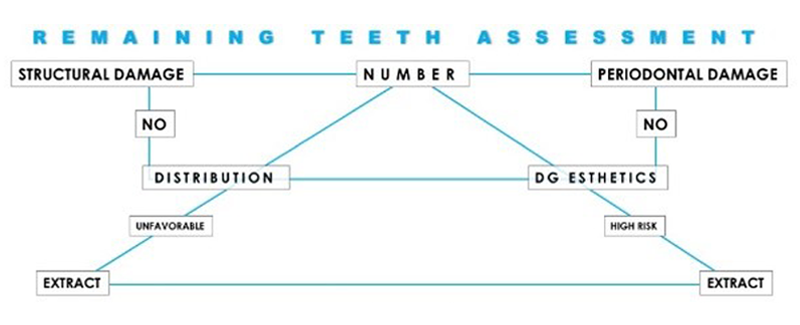
A decision tree, or treatment planning algorithm, can make objective decisions on what should be done with remaining teeth. Decision trees help identify relevant and objective markers that should influence and assist decision-making. This means there will be some evident, undisputable reasons why teeth should be extracted — but it also means there will be some evident, arguable reasons they shouldn’t.
Two undisputable reasons for a full arch extraction of the remaining teeth are:
1. Advanced structural damage (Fig. 1)

2. Advanced periodontal damage. (Fig. 2)

Sometimes not all the remaining teeth present extensive breakdown and still, in the name of a comprehensive or global strategy, it can be decided to remove the remaining teeth that otherwise could be considered worth saving.
But there are three additional contributing reasons to consider:
- The number of remaining teeth
- The distribution of the remaining teeth
- The esthetic challenge that keeping any remaining teeth may pose
Number of Teeth
If four or more teeth remain in one arch and are structurally and biologically sound, the benefit of retaining them needs to be carefully evaluated and considered. (Fig. 3)

Distribution
A relative symmetry of remaining teeth may provide functional and biomechanical advantages that make keeping these teeth worth considering. Also, the strategic position within the arch could make a compelling argument for keeping them. In other words, if there are sound vital intact canines or sound intact canines and molars, it would definitely be worth considering keeping them. (Fig. 4)

Esthetic Challenge
When doing full arch reconstruction, or any reconstruction that includes the anterior or esthetic zone, assessing and keeping the remaining teeth will create an esthetic problem due to aberrantly visible, uneven gingival margins that need to be considered. However, a low lip line situation would favor keeping the remaining teeth. (Fig. 5)

Suppose only a few teeth remain and are structurally and periodontally sound, but their distribution is unfavorable, and they esthetically pose a bigger challenge to manage. In that case, a clinician may strategically remove them to ensure a better outcome. (Fig. 6)

In summary, clinicians consider a patient’s dentition terminal when the risks of retaining the remaining teeth outweigh the benefits of extracting them.
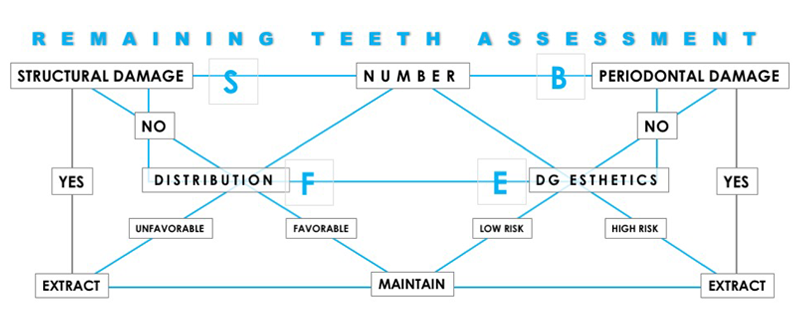
When speaking about these risks, clinicians need to navigate through ESFB risk assessment:
- Esthetic risks
- Functional risks
- Structural risks
- Biologic risks
In the algorithm (Figs. 7-11), the decision process can and should be linear.
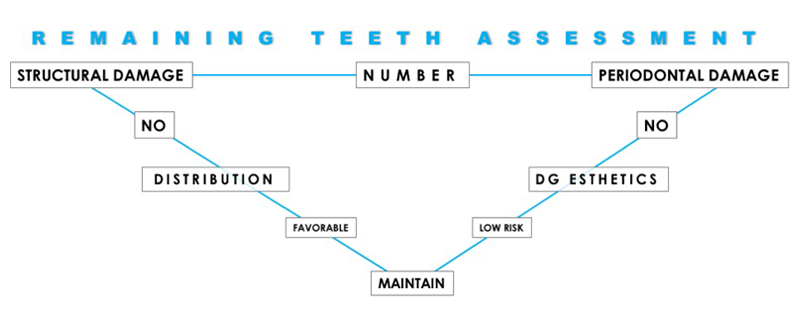
The remaining teeth correlate to all these parameters. But if a patient has a few remaining teeth and their distribution is favorable (i.e., bilaterally symmetric antero-posteriorly; for example, the patient has intact canines and molars), then it would make sense to maintain them.
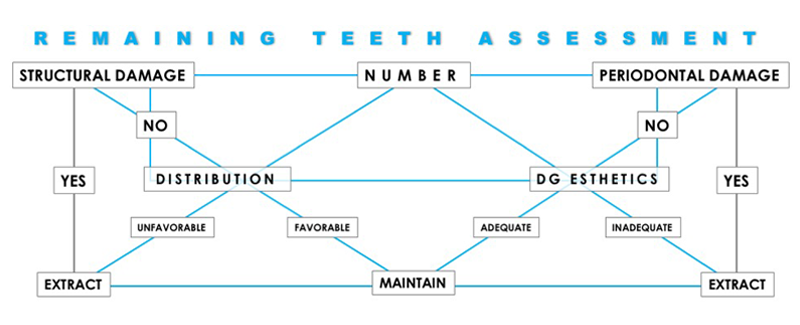
If there is no esthetic risk dento-facially, if the patient has a low lip line, it makes sense to keep some natural teeth, too. Yet if a patient has a few remaining sound teeth, but their distribution is unfavorable (unilateral) and keeping them would pose an esthetic risk, then the indication for extraction is appropriate.
Like any other dentistry area, the decision-making process regarding the preferred therapy should always be contingent upon a patient’s desire, expectations, and financial capabilities. It becomes paramount to utilize a treatment planning framework to review both the clinical and personal aspects to come up with the ideal treatment plan for the patient.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Ricardo Mitrani
Date: June 11, 2019
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


