5 Elements to Consider when Selecting a Full Arch Implant Prosthetic Solution
By Ricardo Mitrani on April 24, 2019 | 2 commentsThe patient population requiring a full arch, implant-supported solution is staggering! As baby boomers age, clinicians need to be prepared to help by considering five essential aspects for the best course of treatment.
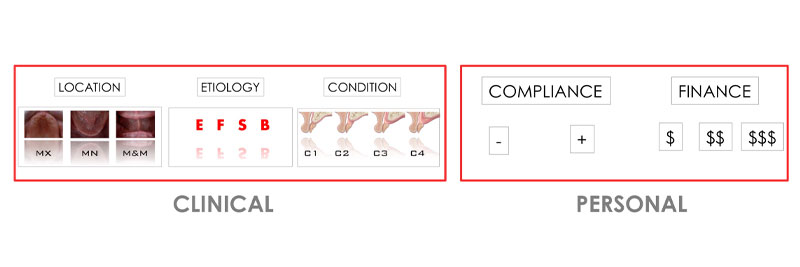
To derive an optimal solution for a patient, the treating team must carefully consider both the clinical and the personal aspects that may influence the case. (Fig. 1)
Clinical considerations
1) Location (Fig. 2)

Treatment planning the maxillary arch is different than treatment planning the mandible. There are differences in bone quality, as well as anatomical limitations, or pitfalls. Also, the level of complexity is different when doing a single arch, as we are limited to treatment plan according to the opposing arch condition as opposed to having full control, either by doing modifications on the opposing dentition, or planning for a full arch solution for both.
There are also treatment planning differences if the patient presents with:
- Terminal dentition
- Healed edentulous arch
- Ill-conceived previous implant-supported restoration
2) Etiology (Fig. 3)

Whether or not some teeth are still present or all teeth are lost and the patient has a healed edentulous arch, the reason behind the loss should be carefully evaluated. The nature of tooth loss has a direct influence not only in the restorative design, but also in the treatment sequence.
Tooth loss can be associated with:
- Structural damage/advanced decay
- Periodontal breakdown
- Trauma/excessive bruxism
3) Condition (Fig. 4)
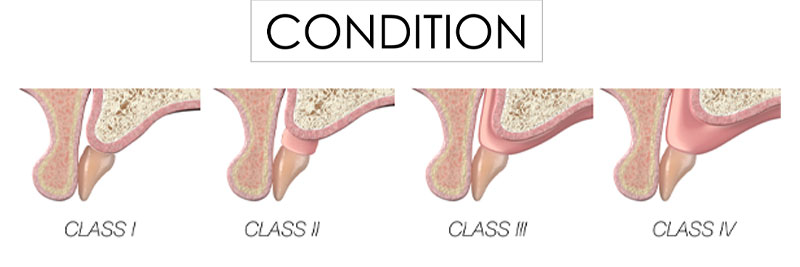
In a previous Spear Digest article, I advocated the importance of implementing the LTR classification in the diagnostic exam because it serves as a guidepost toward selecting the optimal restorative design for patients with either terminal dentition or with a healed edentulous arch.
The LTR classification allows for an objective assessment of the relationship between the optimal tooth position and two anatomical landmarks – the lip and the ridge. By correlating lip mobility, lip support and ridge deficiency, the interdisciplinary team can objectively assign the most appropriate restorative solution based on esthetics, function, structure, biology (EFSB).
Generically, and in the name of simplification, restorative solutions are grouped into:
- Implant-supported overdenture
- Fixed-hybrid design
- Implant-supported fixed dental prosthesis (ISFDP)

Every prosthetic solution has specific space requirements to ensure a long-term, successful performance and prognosis. The restorations may be generically grouped but depending on material selection and sub-system there may be different space requirements (e.g., an overdenture with locators/telescopes needs less vertical space than a bar-and-clip overdenture).
It should also be noted that an LTR Class 1 or 2 patient with a high esthetic risk (HER), high lip mobility is not ideally clinically eligible for a fixed hybrid unless the LTR condition is modified by means of resective surgery. Removing bone to hide the transition line underneath the lip converts the patient from a Class 2 HER to a Class 2 low esthetic risk (LER), while at the same time creating enough space to ensure adequate thickness for optional biomechanics performance of the framework.
This framework allows the team and the patient to easily visualize the biologic price for conversion of the LTR class (bone reduction). Of the same token, it should be noted that selection of a given prosthetic solution is commensurate with the patient's personal preference, behavior and financial capabilities (see below).
Personal considerations
4) Behavioral (Fig. 6)
If the treating team concludes a patient meets every possible clinical parameter needed for an ISFDP, the question now becomes will the patient be compliant with what therapy entails?
Compliance is a word some clinicians advocate to stay away from because it’s deemed politically incorrect. Nonetheless, there must be a consensus from the team regarding if a patient is the right candidate for a given treatment. The concept of compliance is truly a mix of commitment, temperament, motivation, expectations and desire, all of which leads to the patient's ability to cope with all that’s involved with therapy.
Consider a patient with advanced periodontal disease who is an extremely busy business owner, smokes two packs of cigarettes a day, does not show any good signs of home care and regularly cancels their hygiene appointments. Would they be a good candidate if an ISFDP?
5) Financial (Fig. 6)

The next important personal aspect is a patient's financial capability. Solutions can range from an affordable prosthetic design like a locator type of overdenture to a sophisticated solution like an ISFDP, which is usually supported on six or more implants.
After considering all the relevant clinical and personal aspects of a terminal dentition case, the treating team will have a strong framework for implementing successful therapy design.
Ricardo Mitrani, D.D.S., M.S.D., is a member of Spear Resident Faculty.
Comments
May 29th, 2019
May 29th, 2019