Centric Relation to Maximum Intercuspation Slide, Part 1
As dentists, when we see a problem, we see how we can fix it from a tooth-based approach. Admittedly, some of my past patients have been subject to this way of dental treatment.

Asking the bigger questions
But there are many times that one must take a step back and ask the right questions to gain a comprehensive understanding, beyond a single tooth, of the problem at hand. In this article, I will cover the pathological discrepancies between centric relation and maximum intercuspation (also known as centric occlusion) and how this slide can lead to tooth failure.
The triad of function: TMJ, muscles, and teeth
Before we can discuss teeth, we must assess the system in which they work. The system comprises a triad of temporomandibular joint, muscle, and teeth.
Defining centric relation
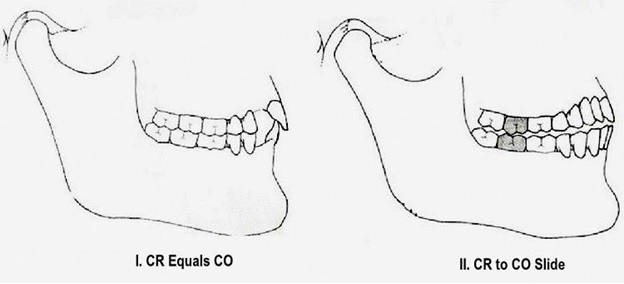
Let’s start with centric relation. There are seven different definitions for CR in the Glossary of Prosthodontic Terms. For the sake of this article, we’ll consider CR as “the maxillomandibular relationship in which the condyles articulate with the thinnest avascular portion of their respective disks with the complex in the anterior superior position against the shapes of the articular eminences.”1
This position is independent of tooth position; the mandible exhibits rotary movement in this position along the transverse horizontal axis; and it is a reproducible position for clinicians. As a clinician, getting the patient into this position is a prerequisite to the analysis of the system. The finishing position in regard to this article is MIP.
Defining maximum intercuspation
Maximum intercuspation is “the complete intercuspation of the opposing teeth independent of condylar position.”1 CR and MIP coincide in only about 10% of the population, leaving 90% of the population to have a slide.1 As a clinician, you must determine if CR is a functioning position and how the patient gets from CR to MIP. Only then can you determine if the slide is pathological or physiological.
When occlusion becomes pathologic
When the teeth, muscles, and joints are able to function independently of one another, the system will remain stable. In a pathologic occlusion, however, “the three elements of the triad are dependent on each other and the powerful muscle engrams accelerate the aging of the teeth and TM joints.”2
The “balanced door” analogy
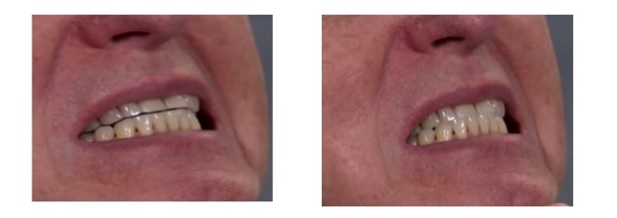
The best analogy I have heard and use with my patients is that the posterior teeth should come together like a perfectly balanced door. As the mandible closes, the TMJs (the hinges) will rotate the mandible so the lower posterior teeth (the door) will fit perfectly into the upper posterior teeth (the frame), allowing the teeth to contact harmoniously and simultaneously.
This is easier said than done, because many pieces have to come together constantly at the right moment to make this perfect closure. If the door closes poorly, drags on the floor, or has to be wedged into the frame, the system will function poorly.2
Few patients have perfect closure
Dr. Pankey notes in his book A Philosophy of the Practice of Dentistry,“I see patients who do not have centric relation occlusion within hollering distance.”2 The point is that very few patients have occlusions that close like a balanced door.
The first point of contact matters
It is essential for the first point of contact to be “one of stability, occurring simultaneously on as many teeth as possible.”2 The contacts should not occur on inclines but instead be a solid stop. Ideally, squeezing the teeth after the first point of contact should not produce any apparent slide to achieve complete closure.
Guidance systems and posterior teeth
Dr. Peter Dawson takes the concept a step further in his textbook Evaluation, Diagnosis, and Treatment of Occlusal Problems by stating: “The occlusal contours of all the posterior teeth are dictated by both condylar guidance and anterior guidance. No posterior tooth should interfere with either anterior guidance or condylar guidance. Posterior teeth may either be discluded from any lateral contact by the anterior teeth, or they must be in perfect harmonious group function with them and the condyles.”2
Signs of a system under stress
The system will start showing signs of stress when condylar, anterior, and incisal guidance become dependent on one another, causing the system to age rapidly in a pathologic fashion. These signs can display as an asymptomatic click in the TMJ, craze lines, abfractions, or soft-tissue irregularities in the periodontium.2
When dependent on each other, the TMJs and the teeth will adapt or age quickly. If the three guidance systems adapt together over time, change can be physiologic, leading to natural aging of the joints and teeth. However, if the guidance systems oppose each other intensely, this will lead to pathologic changes.
References
- Hamdan B. Centric Relation, The Basic Reference. Published October 1, 2014.
- Supple R. Anterior Guidance.
- Christenson G. Ask Gordon: Is there always a shift from centric relation (CR) to maximum intercuspation (MIP)? Published June 27, 2011.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Puneet Sandhu
Date: May 17, 2017
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


