Managing the Midline Diastema, Part 2: Challenges
In the first article in this three-part series, we looked at midline diastemas in terms of etiology, reviewed how to classify them, and walked through the steps of a clinical exam. Now, in this second installment, let’s look at the special challenges that can present when restoring a midline diastema.
Midline diastema cant
How important is this, from an esthetic perspective? Looking at the literature, Thomas1 suggested a midline cant of 10° from the true vertical is perceptible by 41% of the lay (non-dentally qualified) population, whereas Gul-E-Erum and Fida2 found a cant of as little as 5° was noticeable.
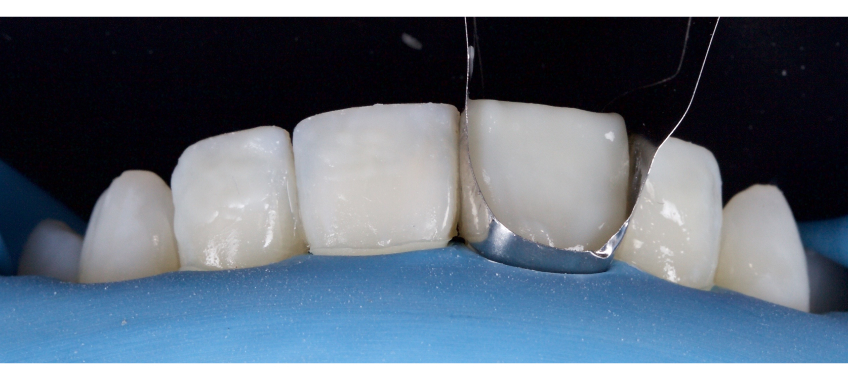
This case I treated (Fig. 1) was a combination of Class IV direct resin restoration of 1.1 with associated Class I diastema closure. An error was made regarding the angulation of the midline, which you can see in the postoperative image.
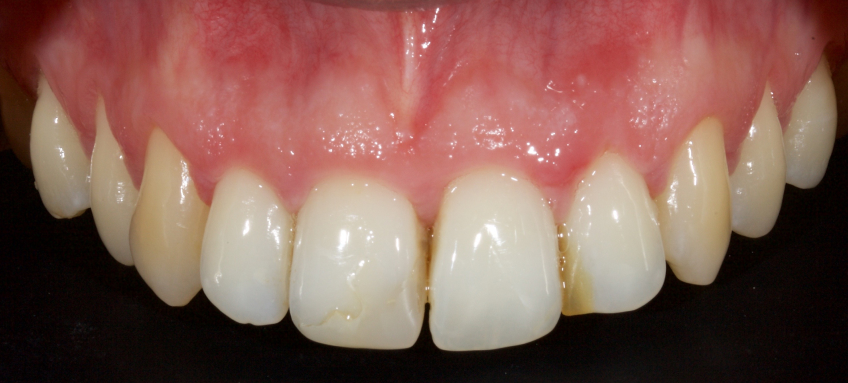

Even though the shade match of the resin was close to perfect and the quality of the polish/finish was high, the patient reattended for correction. This meant patient dissatisfaction, loss of production time, and consequent monetary loss for the office.
Further, you will notice that in isolated two-unit cases such as this, a midline cant also leads to dissimilar widths of the central incisors in the mid and gingival thirds. In my experience, this is the most common reason for re-treatment of diastema closure cases.
Central incisor widths
Every patient is an individual, making selecting optimal dimensions for the teeth challenging.3 Some parameters that are helpful in the design process are:
- Males tend to have larger tooth dimensions than females.4
- The standard width of an upper central incisor is commonly considered to be around 8.5 mm: 8.59 mm for males and 8.06 mm for females.5
However, it should be remembered that these figures relate to Caucasians; widths in Southeast Asia tend to be narrower6 and recently, some authors have reported increased widths of up to 9.24 mm in Caucasian groups in Central Europe.7
Mavroskouvis and Ritchie8 demonstrated that 86%–90% of patients have natural central incisors that are asymmetrical in width; this study showed quite substantial differences, with some subjects having a difference of greater than 1 mm. These findings were confirmed by Chu,9 who also found asymmetry of the order of 0.5 mm between right and left central incisors.
The upper central incisors are the key determinants in assessing the esthetics of the smile: laypeople become less aware of esthetic deviations as you move farther from the midline. For example, small changes in the angulation of upper central incisors are perceived to be unattractive, whereas larger changes (up to 10°) in the angulation of the lateral incisor teeth did not reduce the attractiveness of a smile to a layperson.10
Further, laypeople are more tolerant of wear on lateral incisors than on central incisors,11 and crowding of lateral incisors is less of a concern than crowding of central incisors.12
Finally, eye-tracking studies have demonstrated that when observing the dentition, our first sight fixation is the upper central incisors.13 This suggests that the upper central incisors are the most critical teeth in our smile design.
One of the most important esthetic components of a smile is the symmetry of the teeth, and it is well established that dental professionals are more critical in evaluating the component parameters of a smile than laypeople.14 However, most patients can determine the central incisors’ asymmetry with a “noticeability” cutoff value of 0.2 mm.15
Given the above, the restored central incisors should ideally be the same width with a deviation of less than 0.2 mm. This can be achieved using a dental vernier caliper and the technique described in the final article in this series.
Central incisor proportion in relation to adjacent teeth
Creating a harmonious arrangement of the maxillary anterior teeth can be challenging; to simplify the process, several researchers have suggested mathematical or geometric theories for smile design.16 These are described below.
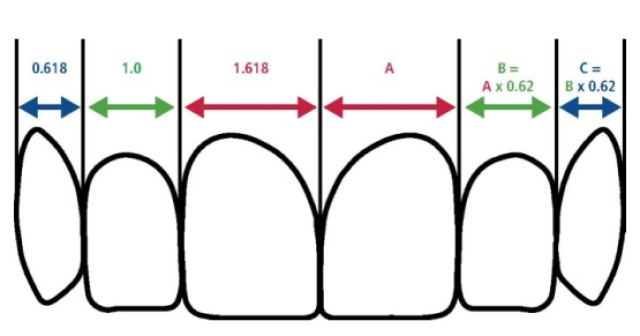
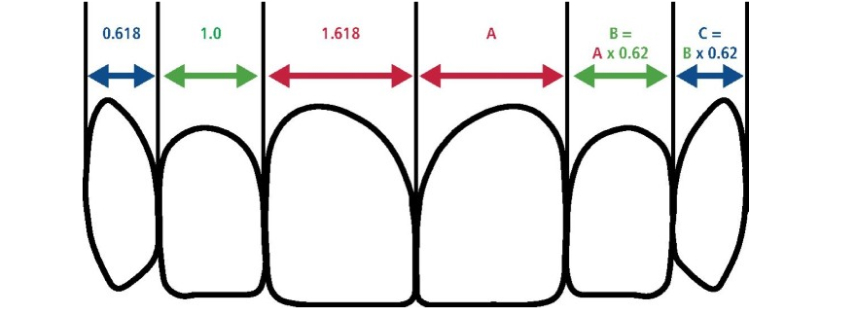
- Levin’s “golden proportion” theory17 states that there is a relationship between mathematics and perceived beauty. Levin suggested that the esthetic ideal has the lateral incisor 0.618 of the apparent width (when viewed from the front) of the central incisor, while the apparent width of the canine should be 0.618 of the apparent lateral incisor width.
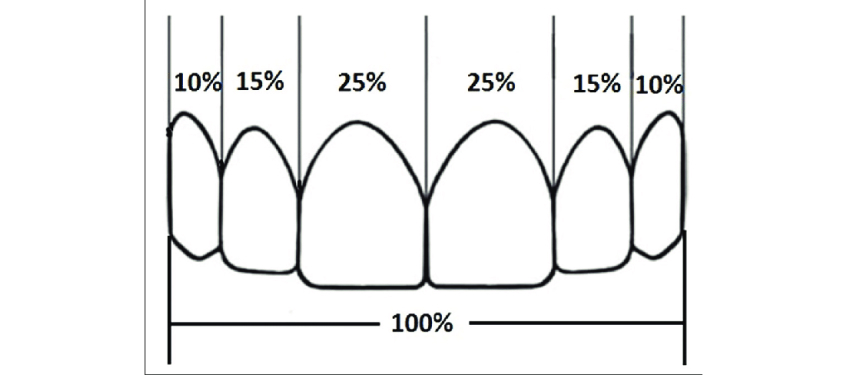
- Snow’s “golden percentage” approach18 asserted that the apparent width of the maxillary central incisor should be calculated as a percentage of canine–canine measurement, with the central incisor, lateral incisor, and canine widths being 25%, 15%, and 10% of the canine-to-canine width.
- Meanwhile, Preston19 suggested that the lateral incisor be 66% of the central incisor width, while the canine be 84% of the lateral incisor width.
I dislike these approaches, because there’s a tendency to make the lateral incisor look rather long and narrow in relation to the central incisors, which results in a “piano key” appearance that appears fake. Personally, I prefer Ward’s “Recurring Esthetic Dental Proportion” theory, which says that the width ratio of two adjacent anterior teeth (e.g., central and lateral, or lateral and canine) should remain the same as one moves distally through the arch. This approach is less rigid than the 62% ratios of the golden proportion, having a range of ratios from 60–80%. The outcome is a more flexible tool to allow the dentist to accommodate dental esthetics into the patient’s facial profile.
When closing a diastema with direct resin as a standalone procedure with no intervention to adjacent teeth, achieving ideal width proportions can be challenging. Often, if the diastema closure is large, the width of the centrals will be excessive and the dimensions of these teeth will be incongruous in the smile. Alternately, with a small diastema closure and teeth that are narrow or quite long — for example, with recession that can’t be managed with periodontal root coverage — the central incisor width may appear narrower than ideal.
I often use optical illusions in these situations to achieve a more esthetic outcome.
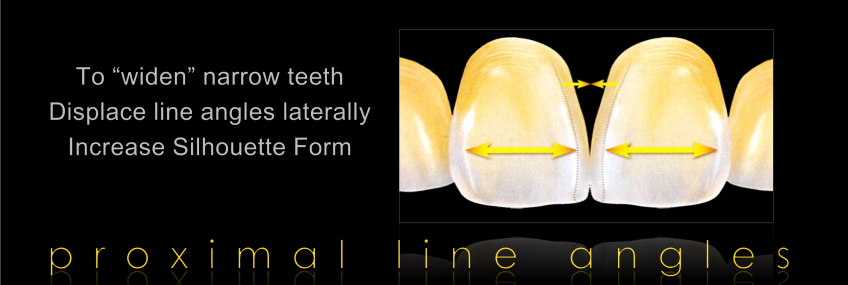
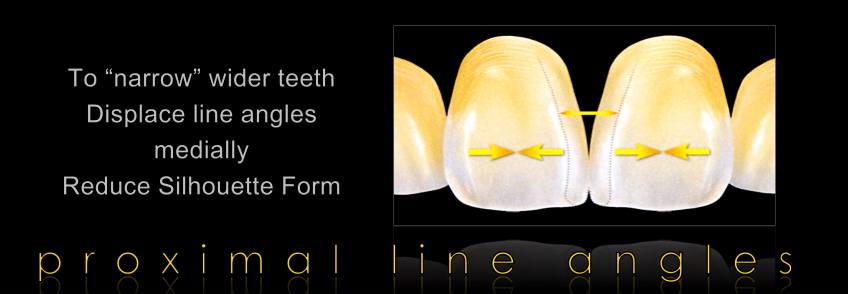
Line angles are the transition points from the interproximal embrasure space to the facial surface: A central incisor has a mesial and distal line angle. The aspect of the tooth mesial to the mesial line angle and distal to the distal line angle tends to be in shadow, while the tooth structure between the line angles (the facial surface) is well lit. More tooth structure catching the light and less in shadow makes the tooth look wider, whereas the opposite is true for the converse.
If the line angles are moved, optical illusions can be used to make the tooth look narrower or wider — i.e., moving the line angles out toward the contact points makes the tooth look wider (Fig. 5), whereas moving the line angles in toward the midline makes the tooth appear narrower (Fig. 6).
Central incisor width-to-length proportion
Tooth width-to-length proportion can be established in several ways:
- Sterret3 measured stone casts and established that the width-to-length ratios of central incisors were around 85% in men and 86% in women.
- Magne7 analyzed extracted teeth and obtained an average value of 78% for the width-to-length ratio of central incisors.
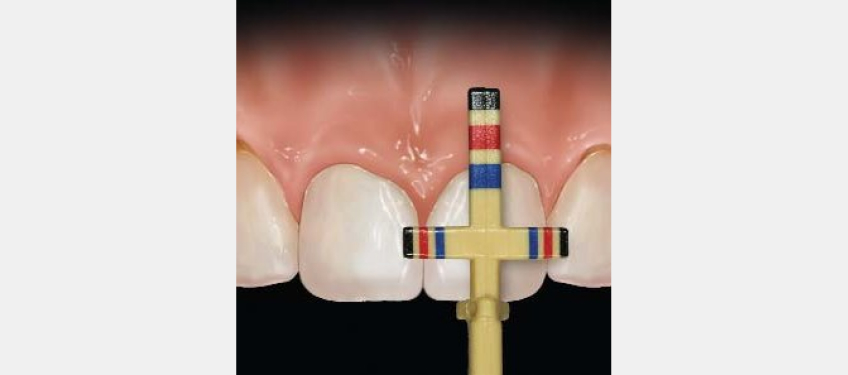
- Chu20 used an innovative measurement gauge (Fig. 7) to optimize esthetics in crown-lengthening procedures; he sets the width-to-length ratio at 78% for all maxillary anterior teeth.
However, it should be remembered that establishing set anterior tooth dimensions with no consideration of variation due to race is illogical, because there are significant variations across different populations.21 Dental esthetics should be designed using anatomical measurements and rules22 that are based on studies conducted within the appropriate population group.23
In my opinion, smile design is an artistic process that should involve the human eye and brain, in conjunction with modern CAD, to achieve a bespoke outcome for each individual.
This can be rehearsed using a diagnostic mock-up and transferred to the mouth with flowable composite resin and a transparent PVS impression of the mock-up. This approach can be used to ensure that both the dentist and the patient are comfortable with the potential outcome.
In the case shown below (Figs. 8–11), the patient presented with a Class II midline diastema and discolored 1.1 and 2.1, further spacing being present mesially and distally to the lateral incisors. An analog wax mock-up was carried out on stone models and transferred to the mouth with flowable composite and clear PVS. At the patient’ s request, the inclination of the lateral incisors was modified in the mock-up phase. This was then copied in the final restoration.




Overhangs
Closure of a midline diastema with direct composite resin is one of the more challenging procedures in restorative dentistry. Other than the dimensional challenges discussed above, a further difficulty is the creation of a smooth, clean transition from tooth to restoration without overhangs. Unfortunately, overhangs are a common challenge (Fig. 12). An overhang is obviously detrimental to periodontal health and is potentially a site for secondary caries. Further, an overhang tends to shred floss and is a common source of patient dissatisfaction.

In terms of matrix systems, there are several options:
- Conventional acetate (mylar strips). This is the most common approach. The disadvantage here is that the strip is flat, and this tends to form a flat triangular emergence profile rather than a more organic rounded profile. In addition, the matrix is challenging to control without wedging.
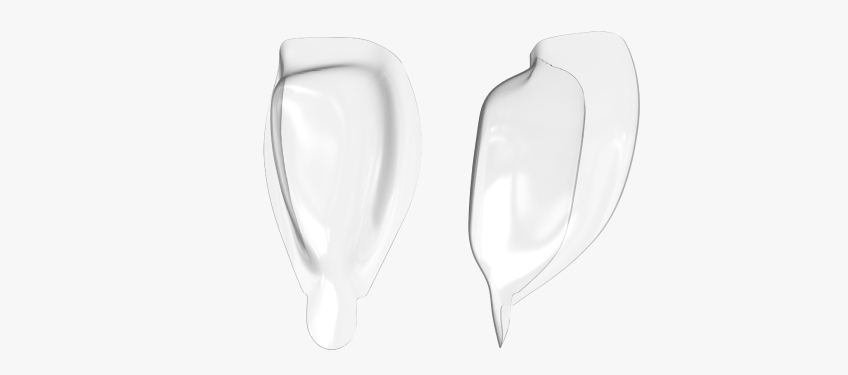
- The Bioclear system. This consists of clear preformed matrices (Fig. 13) of varying sizes and shapes. These are designed for an “injection molding” type of approach — that is, the tooth is restored in one mass with heated low-viscosity composite resin in combination with flowable composite resin. Both central incisors are treated simultaneously. I find these useful for simple diastema closure using one mass of resin. However, for intermediate diastema closure, there are some disadvantages.
- Because of the wraparound design of the matrix, it’s difficult to place an opaque composite resin and a chromatic enamel. In wider diastema closure, there may be some loss of value (graying) of the restoration in comparison to the surrounding tooth structure.
- In a wider diastema, there’s a tendency for the matrix to “tip,” which can result in a canted midline.
- There is often significant excess after injection-molding, resulting in significant finishing procedures.
- Finally, the system involves many matrices, increasing inventory and costs.
- The Unica matrix (Polydentia). This is a metal matrix (Figs. 14 and 15) with a reduced section in the facial and large interproximal “wings.” It can be used for Class III, IV, and V, in addition to diastema closure and restoration of peg laterals. It is relatively simple to use and inexpensive. The downsides I find are that it is sometimes too large in patients with smaller teeth, and the emergence profile tends to be shallow, which often results in a residual black triangle on completion of the closure.

In the case shown in Figs. 16–19, the patient presented with recently placed direct resin closure of her midline diastema and peg laterals. The approach used was an injection molding technique with a clear PVS stent. The resin was failing with generalized staining and fracture of 2.1; large interproximal overhangs were present. The patient did not wish to proceed with orthodontic therapy.
The resin was cautiously removed with a combination of burs, discs, and a #12 scalpel, revealing a challenging space closure. The space was closed with multiple shades of direct resin in combination with Unica matrices. At six-month recall, we can see an acceptable outcome, although a black triangle remains in the midline.




- Sectional posterior matrices. This is the most common approach I use. Conventional sectional posterior matrices are used but rotated by 90° so they]re on their side. The ideal matrix tends to be a heavier gauge (therefore stiffer) and does not have an orientation tab on the concave surface or holes. My preference is for the Garrison M200 or Cosmedent’ s full contact bands. Avoid bands with colored “nonstick” coating because the coating tends to be removed during the procedure, which can contaminate the restoration. The bands can be wedged or secured with Teflon tape at the gingival margin.
Wedging is a further challenge in the procedure. Wedging is desirable to avoid overhangs. However, wedging can create several complications, bleeding being the most obvious issue. A further problem, particularly with wood wedges, is that wedging can create flat, triangular emergence profiles and sometimes even black triangles. Finally, overaggressive wedging can cause irreversible deformation and even papilla loss.
Options for wedging in diastema closure cases are:
- Teflon tape. The Teflon is rolled and packed into the sulcus, pressing the band against the tooth, and closing the margin. The advantages of this approach are a rounded, more organic emergence profile with a minimal risk of black triangles or bleeding. Teflon is economical and has many uses in the dental office. On the downside, it can be challenging to pack Teflon, especially in thin biotype cases. This can be further complicated by the presence of a rubber dam.
- Floss ties. The matrix can be placed between the floss tie and the tooth, using the floss ties to secure the matrix. The advantage is good adaptation of the resin with virtually no risk of bleeding. This approach tends to work best in cases with triangular teeth, where it is easier to pull the floss tie more apically because of the geometry of the tooth.
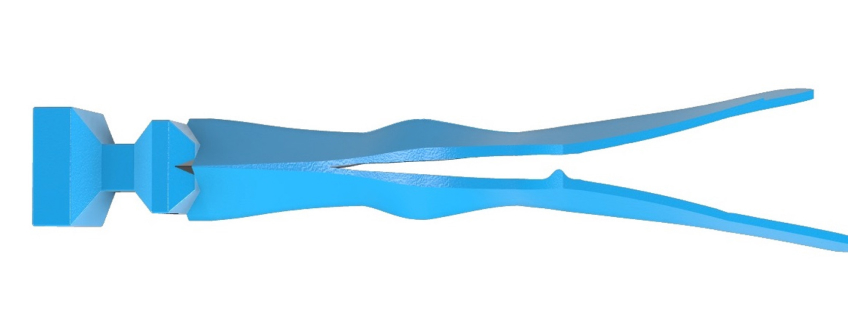
- Vursawedge (BurtonBands). This innovative “split wedge” (Fig. 20) adapts the matrix to the tooth without compressing the papilla apically and causing bleeding. The advantage is excellent adaptation at the margins and a minimal risk of bleeding or papilla loss. There are no significant disadvantages.
This covers most of the significant challenges you may encounter when treating a midline diastema. In the final article in this series, we’ll go through the step-by-step procedure for performing the restoration with direct resin and look at a sample case.
References
- Thomas, J. L., Hayes, C., & Zawideh, S. (2003). The Effect of Axial Midline Angulation on Dental Esthetics. Angle Orthodontist, 73(4), 359-364.
- Gul-E-Erum, & Fida, M. (2008). Changes in Smile Parameters as Perceived by Orthodontists, Dentists, Artists, And Lay People. World Journal of Orthodontics, 9, 132-140.
- Bhuvaneswaran, M. (2010). Principles of Smile Design. Journal of Conservative Dentistry, 13(4), 225-232.
- Alqahtani, A. S., Habib, S. R., Ali, M., Alshahrani, A. S., Alotaibi, N. M., & Alahaidib, F. A. (2021). Maxillary anterior teeth dimension and relative width proportion in a Saudi subpopulation. Journal of Taibah University Medical Sciences, 16(2), 209-216.
- Sterrett, J. D., Oliver, T., Robinson, F., Fortson, W., Knaak, B., & Russell, C. M. (1999). Width/length ratios of normal clinical crowns of the maxillary anterior dentition in man. Journal of Clinical Periodontology, 26(3), 153-157.
- Sah, S. K., Zhang, H. D., Chang, T., Dhungana, M., Acharya, L., & Chen, L. L. (2014). Maxillary anterior teeth dimensions and proportions in a central mainland Chinese population. Chinese Journal of Dental Research, 17(2), 117-124.
- Magne, P., Gallucci, G. O., & Belser, U. C. (2003). Anatomic crown width/length ratios of unworn and worn maxillary teeth in white subjects. The Journal of Prosthetic Dentistry, 89(5), 453-461.
- Mavroskoufis, F., & Ritchie, G. M. (1980). Variation in size and form between left and right maxillary central incisor teeth. Journal of Prosthetic Dentistry, 43(3), 254-257.
- Chu, S. J. (2007). Range and mean distribution frequency of individual tooth width of the maxillary anterior dentition. Practical Procedures & Aesthetic Dentistry, 19(4), 209-215.
- Thomas, J. L., Hayes, C., & Zawaideh, S. (2003). The Effect of Axial Midline Angulation on Dental Esthetics. Angle Orthodontist, 73(4), 359-364.
- Machado, A. W., Moon, W., & Gandini, L. G. (2013). Influence of Maxillary Incisor Edge Asymmetries on the Perception of Smile Esthetics among Orthodontists and Laypersons. American Journal of Orthodontics and Dentofacial Orthopedics, 143(5), 658-664.
- Ma, W., Preston, B., Asai, Y., Guan, H., & Guan, G. (2014). Perceptions of Dental Professionals and Laypeople to Altered Maxillary Incisor Crowding. American Journal of Orthodontics and Dentofacial Orthopedics, 146(5), 579-586.
- Bjelopavlovic, M., Weyhrauch, M., Erbe, C., Burkard, F., Petrowski, K., & Lehmann, K. M. (2021). Influencing Factors on Aesthetics: Highly Controlled Study Based on Eye Movement and the Forensic Aspects in Computer-Based Assessment of Visual Appeal in Upper Front Teeth. Applied Sciences, 11(15), 6797.
- Alomari, S. A., Abu Alhaija, E. S., AlWahadni, A. M., & Al-Tawachi, A. K. (2022). Smile Microesthetics as Perceived by Dental Professionals and Laypersons. Angle Orthodontist, 92(1), 101-109.
- Chrapla, P., Paradowska-Stolarz, A., & Skoskiewicz-Malinowska, K. (2022). Subjective and Objective Evaluation of the Symmetry of Maxillary Incisors among Residents of Southwest Poland. Symmetry, 14(6), 1257.
- Fayyad, M. A., Jamani, K. D., & Agrabawi, J. (2006). Geometric and mathematical proportions and their relations to maxillary anterior teeth. Journal of Contemporary Dental Practice, 7(5), 62-70.
- Levin, E. I. (1978). Dental esthetics and the golden proportion. Journal of Prosthetic Dentistry, 40(3), 244-252.
- Snow, S. R. (1999). Esthetic smile analysis of maxillary anterior tooth width: the golden percentage. Journal of Esthetic Dentistry, 11(4), 177-184.
- Preston, J. D. (1993). The golden proportion revisited. Journal of Esthetic Dentistry, 5(6), 247-251.
- Chu, S. J. (2007). Range and mean distribution frequency of individual tooth width of the maxillary anterior dentition. Practical Procedures & Aesthetic Dentistry, 19(4), 209-215.
- Parciak, E. C., Dahiya, A. T., AlRumaih, H. S., Kattadiyil, M. T., Baba, N. Z., & Goodacre, C. J. (2017). Comparison of maxillary anterior tooth width and facial dimensions of three ethnicities. Journal of Prosthetic Dentistry, 118(4), 504-510.
- Liao, P., Fan, Y., & Nathanson, D. (2019). Evaluation of maxillary anterior teeth width: a systematic review. Journal of Prosthetic Dentistry, 122(3), 275-281.
- Mohammad, A., & Koralakunte, P. R. (2015). Gender identification and morphologic classification of tooth, arch, and palatal forms in Saudi population. Journal of Pharmacy & Bioallied Sciences, 7(2), 486-490.
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!

By: Jason Smithson
Date: December 21, 2023
Featured Digest articles
Insights and advice from Spear Faculty and industry experts