Managing the Midline Diastema, Part 1: Etiology
In this series of three articles, we will look at the midline (or median) diastema between the upper central incisors and its management with direct resin. This first article examines the condition’s etiology and what the initial exams should include. To begin, let’s define our terms:
According to Hussain (Reference 1), a space or gap between two teeth greater than 0.5 mm is called a “diastema”. (Fig. 1)

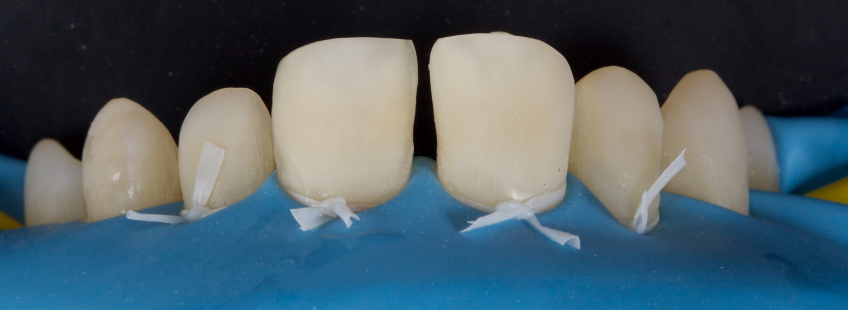
Here, we see a simple diastema with an incongruous direct resin closure that was recently placed. The resin was removed, and the immediate post-op is seen with amore ideal closure and more esthetically integrated direct resin restorations (Figs. 2–4).


Midline Diastema Etiology and Incidence
Midline diastemas are present in 98% of six-year-olds. This figure decreases to 7% of 18-year-olds (Reference 2) because the canines and lateral incisors follow a medial path of eruption, therefore closing the space (Reference 3).
In some people, the diastema does not close spontaneously — and this can be for a variety of reasons.
Historically, the labial frenum was proposed as a primary etiological factor (Reference 4). However, Tait disproved this in the 1930s (Reference 5). Figure 5 shows a large frenum with black triangles but no diastema.

The frenum develops in utero at the tenth week of gestation, extending as a continuous band from the inner of the lip over the alveolar ridge to the palatine papilla.
Before birth, the two halves of the alveolar ridge unite (Reference 6), and this band of tissue becomes enclosed in bone, forming a palatal portion (palatine papilla) and a labial portion (superior labial frenum).
As the child develops, the frenum attachment remains static while bony deposition increases the height of the alveolar ridge. The frenum then appears to migrate apically up the labial surface of the alveolar process. This movement accelerates with the eruption of the permanent maxillary central incisors.
Initially, the maxillary central incisors are flared laterally, meaning a midline diastema is present (“Ugly Duckling Phase”). However, as the lateral incisors and canines erupt, the space is closed, and the frenum atrophies.
Sometimes this does not occur: if both central incisors erupt distant from each other, the rim of bone surrounding each tooth may not extend to the median suture. In this scenario, no bone is deposited inferior to the frenum, and a “V” shaped cleft develops between the two incisors, resulting in an abnormal frenum (Reference 7). Subsequently, transseptal fibers do not proliferate across the cleft, so the space cannot close (Reference 8).
Ceremello (Reference 9) found no correlations between diastema width and frenum attachment, frenum width and diastema, or frenum height and frenum width.
Low and enlarged frena are sometimes seen without a midline diastema; conversely, diastemas can exist without an abnormal frenum. Here, we see my son’s anterior teeth after an unfortunate accident (Fig. 6); you will note a prominent frenum but no diastema.

It is now commonly believed that midline diastemas are usually multifactorial in etiology (Reference 10).
Those factors include:
- Factors associated with normal growth and development. In some subjects, the morphology of the lateral incisors and/or canines may constrain the roots of the central incisors, resulting in a diastema. Also, diastemas are normal in some racial groups that exhibit larger dentoalveolar arches, as we will discuss further on.
- Habits. Specifically, habits that alter the equilibrium between the lips, cheeks, and tongue (for example, digit-sucking and lower lip biting) may result in flaring of the maxillary incisors and a midline diastema.
- Muscular imbalance. When the forces from the extraoral and intraoral soft tissues are unbalanced (for example, development of macroglossia secondary to acromegaly or flaccid lip muscles secondary to lymphangioma), the teeth tend to move until they reach a neutral zone, which is in equilibrium. This commonly results in spacing of the teeth.
- Physical impediment. This is when an object deflects the eruption pattern of the central incisors or moves them laterally to create midline spacing. For example, supernumerary teeth/retained deciduous teeth, persistently enlarged frenum, midline pathology (cysts/fibromas), and foreign body and associated periodontal inflammation.
- Abnormal maxillary arch structure. This results in a large maxillary arch size or bony defects that impede incisor approximation. Examples include open midline sutures, idiopathic midpalatal suture secondary to orthodontic therapy (e.g., rapid palatal expansion), excessive skeletal growth (e.g., with endocrine imbalances), and loss of bony support (e.g., periodontal disease). Here, we see a patient with a midline diastema secondary to reduced periodontal support (Fig. 7).

- Dental Abnormalities. These include abnormal shape, size (Fig. 8), and position of adjacent teeth, including tooth size discrepancies (e.g., peg laterals), missing teeth, and abnormal occlusal relationships (e.g., rotated incisors, Class II, division I malocclusions). This patient presented with a midline diastema and associated peg laterals (Fig. 9). He was comfortable with the spacing, and 1.1 and 2.1 were restored with direct resin (Fig. 10).



Another factor to consider is that there are both racial and gender differences in the incidence of diastemas.
Lavelle (Reference 11) noted a higher incidence in a West African Black population in comparison to White British and Hong Kong/Malay Chinese. Further, Horowitz (Reference 12) reported a significantly higher prevalence in Black Children in comparison to White children (19% vs. 8%). Significantly, Becker (Reference 13) confirmed the racial differences and suggested that in Mediterranean Caucasian and Black subjects, the midline diastema should be considered an ethnic norm.
Although females have a higher prevalence than males up to the age of six, males have a higher prevalence by the age of fourteen (Reference 14).
Diagnosis of the Etiology of the Diastema
A thorough examination should be carried out, and a diagnosis of the etiology of the diastema should be achieved before proceeding with treatment. Failure to do this often results in relapse. Your examination should include the following:
Patient History
Here’s where you discuss:
- Any relevant medical conditions (e.g., hormone imbalance)
- Oral habits (e.g., digit sucking, tongue piercings (Reference 15)
- Previous dental treatment and/or surgeries
- Family history of diastema
Clinical Exam
This is where you evaluate:
- Evidence of oral habits
- Soft tissue balance (e.g., tongue size, lip competence)
- Orthodontic status
- Missing teeth
- Any frenum present, which can be evaluated with the “blanching test.”
Radiographs/Special Tests
Tomograms and periapical radiographs are used to evaluate:
- Dental development
- Midline impediments
- Suture morphology
- Missing teeth
- Dental abnormalities
- Abnormal eruption paths
Performing a Bolton Analysis
Sometimes, full orthodontic records and a Bolton Analysis (Reference 16) are carried out as part of the examination process.
The Bolton Analysis (or Bolton Ratio), described by Wayne A. Bolton, determines the difference in size between the maxillary and mandibular anterior teeth and helps determine the ideal relationship within the interarch.
The analysis measures the relative mesio-distal tooth widths of the upper and lower anterior sextants: clearly, the lower teeth should be smaller than the upper for the lower teeth to fit inside the upper arch and have an ideal molar relationship, overbite, and overjet, in addition to closed proximal contacts without crowding or spacing.
Although the Bolton Analysis can be used for the entire arch, the ratios for the anterior teeth are more commonly employed since anterior tooth size is more variable than posterior tooth size.
The teeth are measured with a Boley Gauge or Vernier Caliper — for example, this product from Great Lakes Dental Technologies (Fig. 11). This can also now be achieved using CAD.

The anterior ratio is 77.2% +/- 1.65: a ratio greater than this suggests the mandibular teeth are larger than usual (and a diastema is more likely), whereas a ratio lower than this means the mandibular teeth are smaller than usual.
Values greater than two standard deviations outside the mean are significant discrepancies.
The values allow clinicians to anticipate the final post-treatment result without the need for diagnostic mock-ups. In the case of diastema closure, a value greater than the mean suggests that the patient will likely need restorative diastema closure even after orthodontic interventions.
It should be remembered that the measurement was made on a Caucasian population, so a drawback is that most populations are not usually “ideal” when compared with the standard ratio (Reference 17). For instance, larger canines, premolars, and first molars are seen in the Black population compared to Caucasians. However, there is no difference in the size of maxillary incisors. Yet there are extensive morphological variations of maxillary incisors between various populations, which are reflected in the Bolton ratio.
In a Brazilian study (Reference 18), tooth size discrepancies were highly prevalent, and this can be explained by the higher degree of genetic mixing in the Brazilian population.
The difference in tooth size between males and females is not similar for all teeth (Reference 19).
Midline Diastema Classification
Diastemas are classified into three categories: simple, intermediate, and complex.
The classification is based on the size of the diastema (the distance between the mesial of one central incisor and the mesial of the other central incisor), which has implications for the treatment chosen.
1. Simple Diastema
Here, the total space is 1.0 mm or less. This scenario best treats with a direct composite since it offers a more conservative solution. There is no preparation other than particle abrasion with 27-micron alumina at a 2-3 bar pressure. The shade of composite used is a chromatic enamel (universal), which matches the tooth structure to be restored. For a discussion on composite selection, refer to this article.

2. Intermediate Diastema
In this classification, the total space is 1.0-3.0 mm. The restoration options are either direct composite or ceramic veneers. The ceramic veneer will require a subgingival preparation and breaking the contact areas to achieve the correct emergence profile: this may be acceptable in the presence of existing Class III or Class IV restorations. (Fig. 13)

This patient (Fig. 14) presented with peg laterals and a midline diastema. The direct resin restorations that I placed about 15 years previously, when she was in her mid-teens, were failing — the centrals had fractured secondary to trauma, and the diastema had opened secondary to growth. The patient chose ceramic veneers.

The teeth were prepared (Fig. 15) — note the degree of wrap-around to create an ideal interproximal emergence — and final ceramic veneers were placed (Fig. 16). However, for virgin teeth, I prefer a direct resin approach since it is less destructive.


This patient (Fig. 17) presented with pathway wear and a relapsed resin diastema closure. After equilibration, the resin was removed (Fig. 18), and the diastema was closed with direct resin — the four-year (Fig. 19).



3. Complex Diastema
In this classification, the space between teeth is greater than 3.0 mm. Unless the tooth’s length is increased significantly, it is usually challenging to create an acceptable width-to-length ratio. Typically, these cases require orthodontics in conjunction with restorative strategies.
This patient (Fig. 20) presented with a complex midline diastema. Following orthodontics, she was ready for restorative care (Fig. 21). Occasionally, this kind of case can be treated restoratively without orthodontics if significant tooth surface loss is present, and the diastema is treated with other teeth in the arch. Typically, this takes the form of an FMR with ceramics.


I hope you have gained a more nuanced understanding of midline diastemas, the etiology behind the condition, and how to categorize the cases you see. In the following article in this series, we will look at the unique challenges you might face during treatment.
References
- Merz, M. I., & Isaacson, R. J. (1991). Tooth Diameters and Arch Parameter in a Black and White Population. American Journal of Orthodontics, 100, 53-58.
- Hussain, U., Ayub, A., & Farhan, M. (2013). Etiology and Treatment of Midline Diastema: A Review of Literature. Pakistan Orthodontic Journal, 5(1), 27-33.
- Foster, T. D., & Grundy, M. C. (1986). Occlusal Changes from Primary to Permanent Dentitions. Journal of Orthodontics, 13, 187-193.
- Broadbent, B. H. (1937). The Face of the Normal Child (Diagnosis, Development). Angle Orthodontist, 7, 183-208.
- Sicher, H. (1952). Oral Anatomy (2nd ed.). The CV Mosby Co: St Louis, pp. 185, 272-3.
- Tait, C. H. (1934). The Medium Fraenum of the Upper Lip and Its Influence on the Spacing of the Upper Central Incisor Teeth. Dental Cosmos, 76, 991-992.
- Dewel, B. F. (1966). The Labial Fraenum, Midline Diastema and Palatine Papilla: A Clinical Analysis. Dental Clinics of North America, 10, 175-184.
- Ferguson, M. W. J., & Rix, C. (1975). Pathogenesis of Abnormal Midline Spacing of Human Central Incisors. A Histological Study of the Involvement of the Labial Fraenum. American Journal of Orthodontics, 67, 139-158.
- Campbell, P. M., Moore, J. W., & Matthews, J. L. (1975). Orthodontically Corrected Midline Diastemas. A Histologic Study and Surgical Procedure. American Journal of Orthodontics, 67, 139-158.
- Ceremello, C. J. (1933). The Superior Labial Fraenum and the Midline Diastema and Their Relation to Growth and Development of the Oral Structures. American Journal of Orthodontics, 39, 120-139.
- Huang, W. J., & Creath, C. J. (1995). The Midline Diastema: A Review of its Etiology and Treatment. Journal of Pediatric Dentistry, 17(3), 171-179.
- Lavelle, C. L. (1970). The Distribution of Diastemas in Different Human Population Samples. Scandinavian Journal of Dental Research, 78, 530-534.
- Horowitz, H. S. (1970). A Study of Occlusal Relations in 10-12-Year-Old Caucasian and Negro Children: Summary Report. International Dental Journal, 20, 593-605.
- Becker, A. (1977). The Median Maxillary Diastema: A Review of Its Etiology. Israeli Journal of Dentistry and Medicine, 26, 21-27.
- Richardson, E. R., Malhotra, S. K., Henry, M., & Coleman, H. T. (1973). Biracial Study of the Maxillary Midline Diastema. Angle Orthodontist, 43, 438-443.
- Rahilly, G., & Crocker, C. (2003). Pathological Migration: An Unusual Cause of Midline Diastema. Dental Update, 30(10), 547-549.
- Bolton, W. A. (1962). Clinical Application of Tooth Size Analysis. American Journal of Orthodontics, 48, 504-528.
- Ebadifar, A. (2013). Comparison of Bolton’s Ratios Before and After Treatment in an Iranian Population. Journal of Dental Research, Dental Clinics, Dental Prospects, 7(1), 30-35.
- Araujo, E., & Souki, M. (2003). Bolton Anterior Tooth Size Discrepancies Among Different Malocclusion Groups. Angle Orthodontist, 73, 307-313.
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Jason Smithson
Date: December 14, 2023
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


