Dental Quality Assurance Using Plan, Do, Study, Act (PDSA), Part 1
Improving the level of care provided to your patients is at the forefront of most dental professionals. Continuing education courses and collaborating with peers are ways to learn new techniques and enhance your skills. Incorporating the scientific principles used in other health care settings to advance the quality of clinical care you provide will also improve patient outcomes. Many dental quality assurance activities can be applied to your clinical processes, ultimately improving the patient experience and adding more value to your practice.
The process of dental quality assurance originated in the manufacturing world, where efficiency and reducing costly errors are key to successfully competing in local, regional, and global markets. The techniques have been adapted to meet the needs of complex systems where multiple systems or teams are present as part of the overall process. No matter what outcome you seek to improve, one question always needs to be answered: how will you know when you have reached your desired goal or objective?
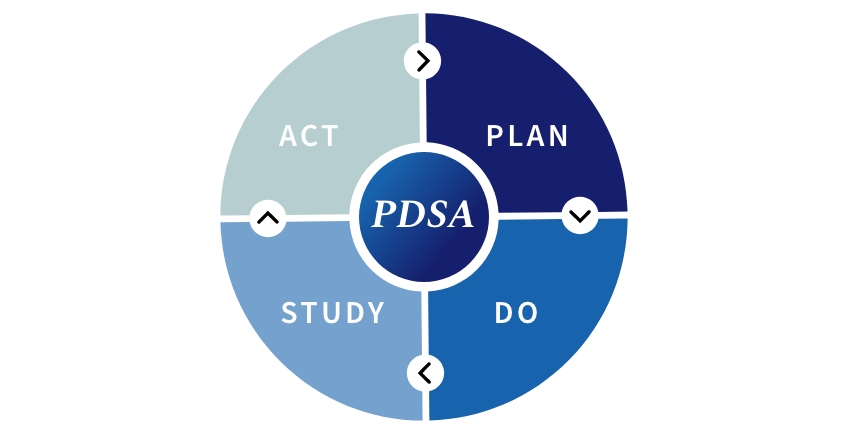
A system that I have used for years in my clinical practice and in our dental laboratory is the Plan, Do, Study, Act (PDSA) model (Fig. 1). It is adaptable to any quality issue you may want to address and is very simple to implement. It provides a structure to figure out what is behind the problem, is interactive (you can pull in your colleagues or assistant to help you brainstorm), and is inclusive. It uses quantitative measures to define your goals, outcomes, or quality improvement parameters. The planning stage is the first part, and the most important, as it sets up your entire process.
Dental Quality Assurance Plan, Do, Study, Act (PDSA) Model
Step 1: Plan
Define the Problem
Do not assume you know why you cannot reach your clinical goal. You need to determine where the problem exists by doing an unbiased and comprehensive analysis. Get input from as many people as you can. Consult colleagues, trusted mentors, and your dental/interdisciplinary team members to help you brainstorm. I think you’ll want to start this process with a clear end goal in mind.
Let’s start with this as an example. Assume you have a problem bonding only veneer indirect restorations (crowns or other partial coverage restorations are not a problem). Clearly identifying when or where the problem occurs and any contributing factors is essential. You also need to identify all the stakeholders (who are all involved or affected by the problem) and how they may contribute to the issue being addressed.
Why is there only a problem when bonding veneer restorations? Is it only when using a specific dental restoration material, or is it with all your materials? Do you not know the correct bonding protocol for the restoration type being inserted or the bonding system used? Is it a patient issue or a clinician issue?
It is important to investigate and include as many specific underlying details and causes of the problem as possible.
Identify the Desired Outcome
It’s not enough to say you want all the restorations to bond appropriately at the insertion appointment. You need to know what you want to accomplish and the timeline. The outcomes should be measurable and specific. For example, all veneer restorations I insert will bond according to expectations by December 31.
Determine the Steps Needed to Reach Your Outcome
Then determine what steps you need to reach your desired goal or outcome.
- List and analyze all the steps in the current process (a cause-and-effect diagram is excellent for this)
- Identify all the stakeholders who are involved in the process. It’s essential that whoever is involved in solving the problem is involved in the problem identification and outcome planning process
- Determine what data/information you need to collect
- Decide how you will collect and analyze the data
- What is the current baseline (20% bond without difficulty? 50%? None?)
- Establish what steps you need to take and the timeline for the change.
Cause and Effect Diagram
To help you clearly define the problem, you need to determine the causes and effects of your current system of bonding the restorations to get to the root cause of the problem. My favorite root cause analysis tool is the fishbone diagram (Fig. 2). It’s called that because a completed diagram can look like the skeleton of a fish. You can draw it out on a piece of paper or whiteboard with input from your colleagues, office staff, or dental technician/lab, or use an online template.
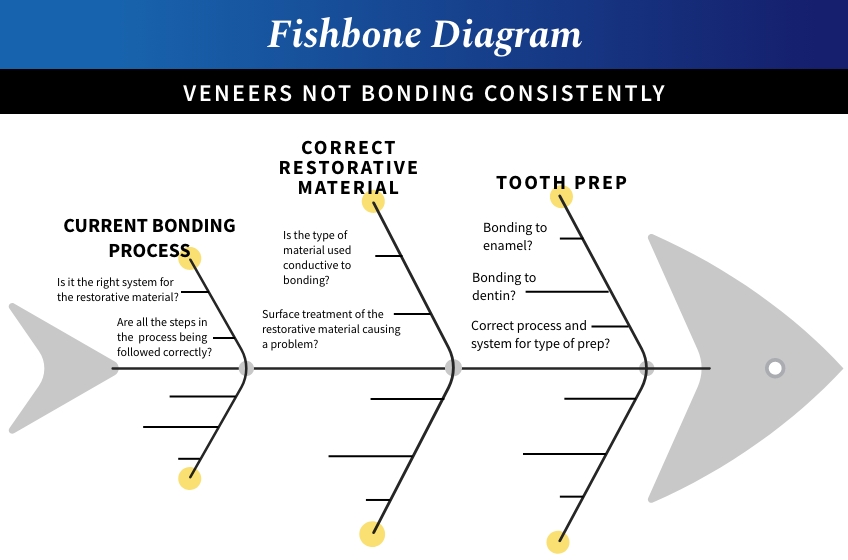
If doing it without a template:
- Write the problem in a box on one end of the paper or whiteboard (veneers restorations not bonding consistently)
- Draw a line horizontally from the box (this looks like the head and spine of a fish)
- Draw lines off the spine for each factor that is contributing to the problem, and label it.
- This can include people involved with the problem, systems, equipment, materials, external forces, etc. In the example I provided, I only listed three: the bonding process, restorative material, and tooth prep. I am sure you can think of others.
- Try to draw out as many factors contributing to the problem as possible.
- For every factor you listed, could you write out all the possible causes for why you cannot consistently bond veneer restorations? I listed two or three in the example, but you may have more, depending on how deep you dive.
- Now you can sit back and analyze what you have documented. Depending on the complexity of the issue/problem, you can now dig even further. You may need to contact outside vendors, your lab, patients, etc. Sometimes, surveying with your peers to see what works in their practice is helpful.
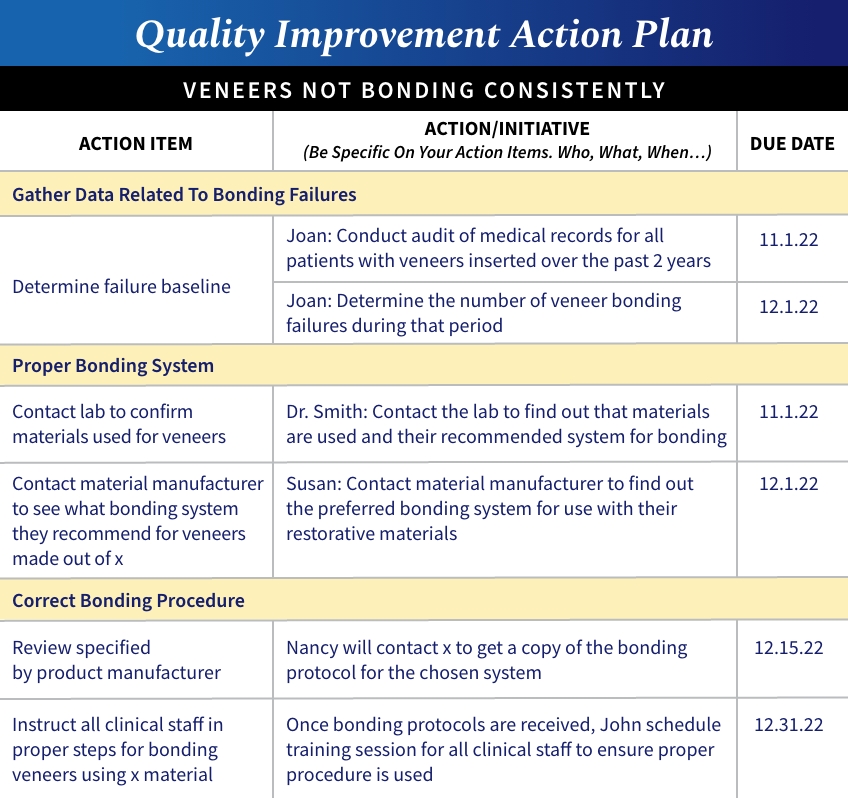
Establish a Plan
Once you have identified the potential causes of the problem, the next step is to develop a plan to improve the process.
For example, if the bonding system you are using is appropriate for the restorative material being used, try to identify what steps in the process, from preparation to the restoration’s return from the laboratory, may be the root of the problem. Once that is done, it’s essential to determine exactly what you will do, who will do it, and the target completion date. Just like when you went through the process to determine the cause of the problem, the plan should be detailed and specific.
An example of a detailed action plan (Fig. 3). Making a similar chart and posting it where everyone involved can see it helps keep everyone accountable for finding the solution.
Hopefully, you will find this helpful when determining why you are not meeting your clinical goals, and it will help you improve the quality of the care you provide to your patients. Remember, do not assume you know what the cause of the problem is. When people reach out to discuss a clinical problem, the underlying reason is often not what the person thinks it is. In the final part of this article, I will discuss the Do, Study, and Act portion of the PDSA quality assurance process.
SPEAR NAVIGATOR
Transform how your practice runs by engaging the team through
coaching and training
A guided path to excellence through structured coaching and self-guided resources that will align your team, streamline processes and drive growth. Transform your practice by implementing Spear’s proven playbooks for developing and retaining a high-performing dental team.

By: Robert Winter
Date: December 1, 2022
Featured Digest articles
Insights and advice from Spear Faculty and industry experts



