A Digital Approach to Occlusal Appliance Fabrication
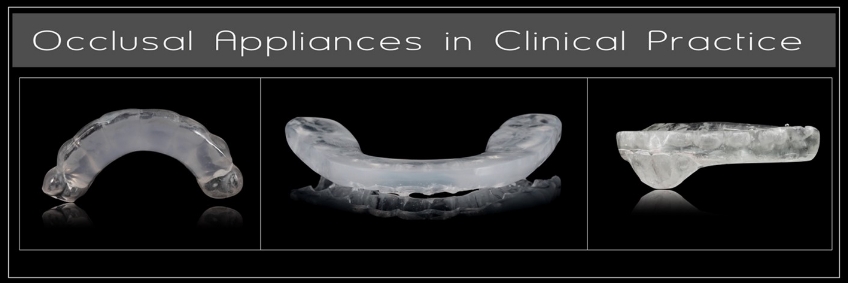
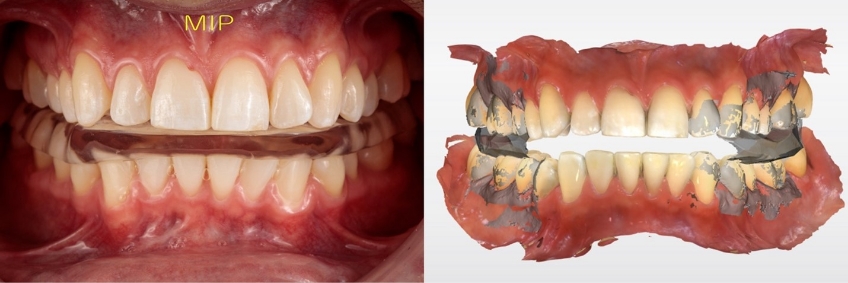
Occlusal appliances are frequently used for diagnostic, therapeutic, or protective purposes. Depending on the goal for an occlusal appliance, a specific design will be prescribed, including the selected arch, maxillary-mandibular relationship, and the desired occlusion (Fig. 1). Analog approaches are well documented. Still, increasingly, a digital approach to occlusal appliance fabrication is becoming more popular due to reduced costs and desired results.
Digital Approach to Occlusal Appliance Fabrication: Three Components
Classically, occlusal appliances have been fabricated from gypsum casts. While the analog approach is time-tested and can produce an occlusal appliance that fits well to the teeth and requires minimal occlusal adjustment at the time of insertion, it is also time-consuming for the clinician to acquire the clinical information and for the technician to fabricate the appliance.
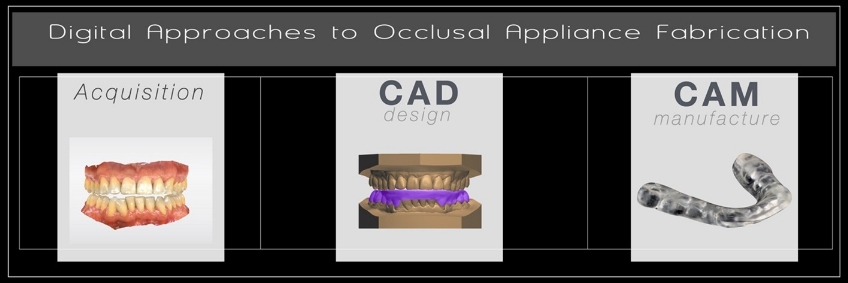
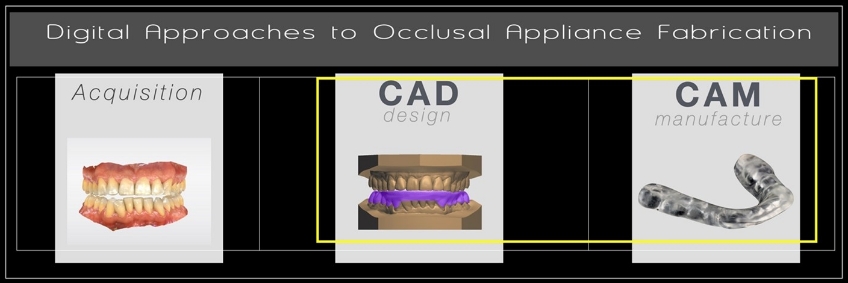
With the rapid increase in clinicians using chairside digital scanning technologies, a digital approach to occlusal appliance fabrication is increasingly common, and workflows are emerging. As with all digital approaches to fabrication, the process may be broken down into three main components: acquisition, design, and manufacture (Fig. 2).
When most clinicians imagine a digital approach to occlusal appliance fabrication, they picture beginning the process with direct, chairside scanning of the patient. This is the acquisition stage. While it is undoubtedly possible to scan an analog cast or even an analog impression, doing so would limit the potential for improved efficiency with the direct digital approach. Accurate acquisition of the patient’s clinical information is a key first step in fabricating an accurate occlusal appliance.
CAD (computer-aided design) — the digital design stage of appliance fabrication — is the most overlooked of the three components. Before any manufacturing process begins, a design for the appliance must be developed. This design step should follow the clinician’s selected appliance design; it most closely follows the waxing stage of an appliance in an analog approach. Therefore, CAD requires specific software and associated learning curves for clinicians and is the last step clinicians decide to perform in-house. (As an interesting side note: manufacturers and developers are hopeful that occlusal appliance design will soon be successful using artificial intelligence. SprintRay and 3Shape both currently offer A.I. designs for occlusal appliances.)
The third and final component in the digital fabrication process is actual manufacturing, or CAM (computer-aided manufacturing). Early digital approach to occlusal appliance fabrication used a subtractive manufacturing process by milling a pre-polymerized puck and a large five-axis laboratory milling unit. However, milling acrylic resins is a slow process and is increasingly being replaced by additive manufacturing in dental laboratories and clinical practices. Since clinicians have already invested, or are considering investing, in desktop 3D print technology, occlusal appliances are a natural fit for in-house manufacture.
The following case illustrates how these concepts come together in a digital approach to occlusal appliance fabrication.
Clinical Example with Digital Fabrication
In this clinical example (Fig. 3), a middle-aged male patient has been prescribed a protective occlusal appliance. The design selected is a full-coverage appliance for the lower arch with little to no steepness to the anterior guidance (often described as a “flat plane”). The appliance will have an occlusion developed with the condyles in a seated position (centric relation).
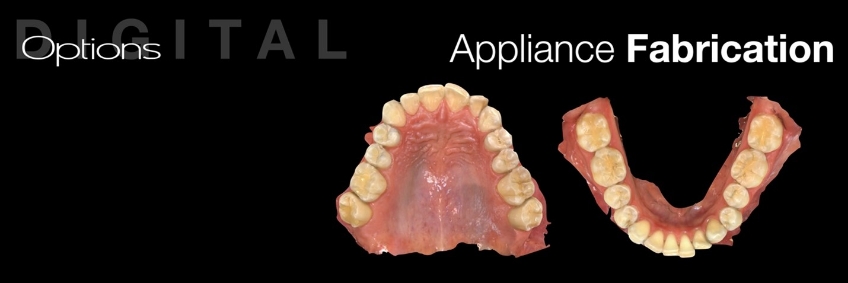
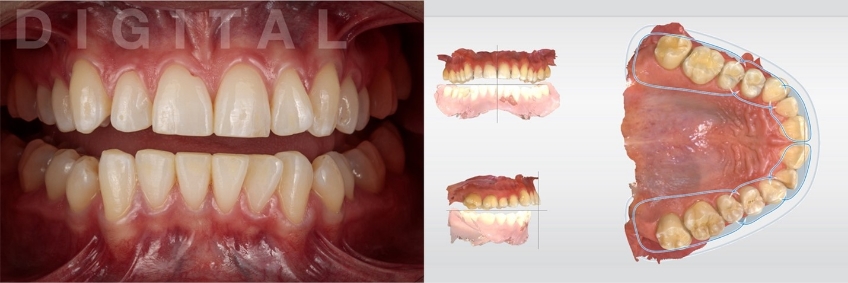
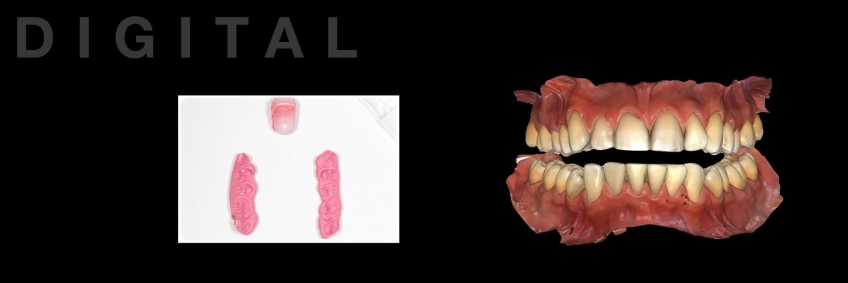
Clinical information collected during acquisition must be accurate for the definitive occlusal appliance to fit well to the patient’s teeth, and a minimum adjustment must be made at the insertion appointment. Both arches were scanned directly following the manufacturer’s instructions (Figs. 4 and 5).

Since the selected appliance is to function from a fully seated condylar position, the interocclusal record must capture the inter-arch relationship in this condylar position. In a fashion like what was described in my previous article on analog fabrications, the condyles are seated using a Lucia jig (Great Lakes Dental Technologies, Buffalo, New York). For this patient, the prefabricated Lucia Jig increased the occlusal vertical dimension sufficiently to allow for a minimum of 2.0 mm of occlusal appliance material thickness. A leaf-gauge or bimanual approach could also have been used (Fig. 6).
Following a direct scan of both arches and fabrication of the interocclusal record at the desired occlusal vertical dimension, the jaw relationship was digitally acquired as the “buccal bite.” During this step, the silicone bite segments were left between the posterior teeth while scanning to minimize the risk of mandibular movement. The anterior deprogrammer is inconsequential for this step and was removed before scanning. In some cases, the buccal aspect of the bite registration material may need to be trimmed so that the chairside scanner can detect enough common points to allow the files to stitch (Fig. 7).
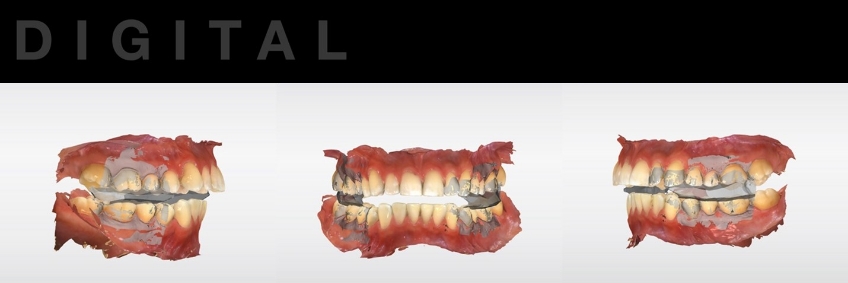
Since the interocclusal relationship was determined and recorded clinically, there should be little to no need to alter the occlusal vertical dimension in the virtual articulator. Minimizing alterations to the pin setting will also minimize the introduction of error into the case. Should the occlusal vertical dimension require alteration, clinicians should anticipate the possibility of increased occlusal adjustment at the insertion appointment (Fig. 8).
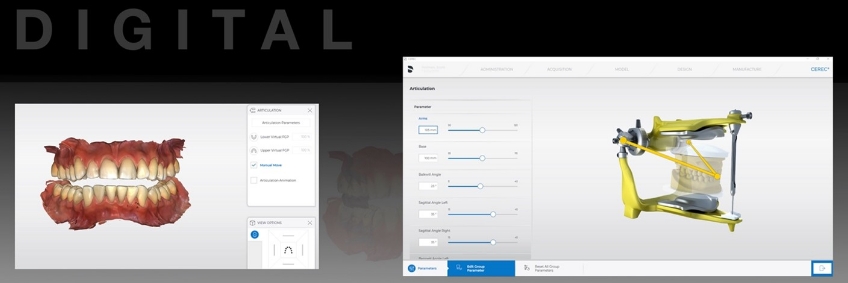
The acquired clinical information may be transferred to the technician and the prescribed appliance design. While technology is required, specifically a chairside scanner for acquisition, the design and manufacture are now outsourced to the dental technician. An advantage to this approach is that no clinical staff time is required for either CAD or CAM, making it a great entry point for clinicians not currently printing in their offices (Fig. 9).
The technician will design the appliance digitally and complete the digital manufacturing using a milled approach. This approach closely follows the concepts clinicians are familiar with from analog occlusal appliance fabrication (Figs. 10-13).
Alternatively, the case design can be outsourced, and the design file returned to the clinician for in-house manufacturing. This approach is increasingly common with practitioners interested in desktop 3D printing but who do not want to spend time designing the case. Should a clinician want to exert full control over digital fabrication, several design software programs are available.



Why it Pays to Get this Right
With assorted designs and goals, occlusal appliances are common treatment options in many clinical practices. Since they are so common, small improvements in predictability and efficiency can add up to large savings over a year.
While it may seem overly labor-intensive to virtually articulate casts with precise accuracy when fabricating something as ubiquitous as a protective occlusal appliance, the investment in time and effort spent during the acquisition phase is returned at the time of insertion in the form of minimal need for occlusal adjustment. A digital approach to occlusal appliance fabrication is the future.
References
- Zonnenberg, A. J., Türp, J. C., & Greene, C. S. (2021). Centric relation critically revisited—What are the clinical implications? Journal of Oral Rehabilitation, 48(9), 1050-1055.
- Bidra, A. S., Daubert, D. M., Garcia, L. T., Kosinski, T. F., Nenn, C. A., Olsen, J. A., … & Curtis, D. A. (2016). Clinical practice guidelines for recall and maintenance patients with tooth-borne and implant-borne dental restorations. The Journal of the American Dental Association, 147(1), 67-74.
- Chen, H. M., Liu, M. Q., Yap, A. U. J., & Fu, K. Y. (2017). Physiological effects of anterior repositioning splint on temporomandibular joint disc displacement: a quantitative analysis. Journal of Oral Rehabilitation, 44(9), 664-672.
- Kashiwagi, K., Noguchi, T., & Fukuda, K. (2021). Effects of soft occlusal appliance therapy for patients with masticatory muscle pain. Journal of Dental Anesthesia and Pain Medicine, 21(1), 71.
- Kattadiyil, M. T., Alzaid, A. A., & Campbell, S. D. (2021). What materials and reproducible techniques may be used in recording centric relation? Best evidence consensus statement. Journal of Prosthodontics, 30(S1), 34-42.
- Koppolu, S. K., & Manoharan, P. S. (2022). Shifting focus from subtractive to additive technology in digital prosthodontics. SRM Journal of Research in Dental Sciences, 13(2), 74.
- Li, J., Chen, Z., Dong, B., Wang, H. L., Joda, T., & Yu, H. (2020). Registering maxillomandibular relation to create a virtual patient integrated with a virtual articulator for complex implant rehabilitation: a clinical report. Journal of Prosthodontics, 29(7), 553-557.
- Lepidi, L., Chen, Z., Ravida, A., Lan, T., Wang, H. L., & Li, J. (2019). A full‐digital technique to mount a maxillary arch scan on a virtual articulator. Journal of Prosthodontics, 28(3), 335-338.
- Nagy, W. W., & Goldstein, G. R. (2019). Facebow use in clinical prosthodontic practice. Journal of Prosthodontics, 28(7), 772-774.
- Nazir, O., Singh, R., Tantray, M. A., & Farhaan, M. (2021). Occlusal appliance therapy: A review. IP Annals of Prosthodontics and Restorative Dentistry, 7(2), 84-86.
- Piskin, B., Uyar, A., Yuceer, M., Topal, S. C., Senturk, R. A., Sutcu, S., & Karakoc, O. (2021). Fabrication of a mandibular advancement device using a fully digital workflow: a clinical report. Journal of Prosthodontics, 30(3), 191-195.
- He, Shushu, Si Wang, Fang Song, Shu Wu, Jiangyue Chen, and Song Chen. “Effect of the use of stabilization splint on masticatory muscle activities in TMD patients with centric relation-maximum intercuspation discrepancy and absence of anterior/lateral guidance.” CRANIO® 39, no. 5 (2021): 424-432.
- Solow, R. A. (2013). Customized anterior guidance for occlusal devices: Classification and rationale. The Journal of Prosthetic Dentistry, 110(4), 259-263.
- Wiens, J. P. (2016). A progressive approach for the use of occlusal devices in the management of temporomandibular disorders. General Dentistry, 64(6), 29-36.
- Wu, K., Dominici JT. (2020) Desktop 3d printing for occlusal splints. Decisions in Dentistry, 6(5), 14-17.
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Darin Dichter
Date: November 17, 2022
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


