Loading Protocols for Implant Overdentures: To Wait or Not to Wait?
For patients missing all their teeth in one or both arches, there have never been more options available for replacing those teeth than today. The literature and clinical experiences are full of reports of positive patient outcomes utilizing dental implants to improve comfort, function, and appearance.
A variety of prosthetic options exist to help support our patients with one or both edentulous arches, but there is no universal implant number or position that will work for every design. Therefore, prosthetic planning must be well thought out before the dental implants are placed.
With the wide range of prosthetic options available, many questions arise. Some are specific to sequencing the treatment with a particular design, while others may be more general. For any designs that utilize implants, one could ask: How soon can you load implant overdentures?
This is an excellent question in a practice landscape where patients may expect “teeth in a day”! Let’s explore this question in-depth.

Defining Loading Protocols
The original Branemark loading concepts suggested submerging dental implants for three to six months before uncovering the fixtures and attaching them to a dental prosthesis.
This conservative concept was conceived largely empirically and was designed to avoid micromotion of the still-integrating implants and the resulting introduction of a connective tissue layer at the implant-bone interface (i.e., failure to osseointegrate).
Modern loading protocols have evolved along with implant design and surface technology. While some discussion remains regarding loading protocols, many researchers and clinicians follow these general guidelines for describing the timing of implant loading:
Conventional Loading
The prosthesis is attached to dental implants two months or more after implant placement.
Immediate Loading
The prosthesis is attached to dental implants for one week or less following implant placement.
Early Loading
The prosthesis is attached to dental implants between one week and two months following implant placement.

Fixed vs. Removable
Immediate loading is well documented (Papaspyridakos et al. 2014) in the maxilla and the mandible when using a fixed dental prosthesis. The cross-arch stabilization of the fixed prosthesis is effective in sufficiently reducing micromovement of the integrating implants. As a result, immediate loading is an approach that should be considered for a fixed reconstruction on dental implants.
Far less is understood regarding the influence of implant loading protocols when implant overdentures are being utilized. Confusion about appropriate loading times with overdentures is understandable within the context of the risk to osseointegration from micromovement, considering that the implants will be subject to significant loading both under function and when the prosthesis is removed and inserted. The confusion is then amplified when the heterogeneity of overdenture design is considered.
As a result, the question is: “Which loading protocol should be utilized when the dental implants are attached to a removable prosthesis, or overdenture?”
To answer that, the current literature is quite helpful.
Loading Protocols for Implant Overdentures: A Systematic Review
In a 2021 systematic review and meta-analysis, Borges et al. looked at long-term outcomes of different loading protocols when implant overdentures replaced missing teeth in the mandible.
The authors concluded that success in the mandible. Further, given the benefits of shortened overall treatment time, immediate and early loading protocols should be considered in clinical practice.
Cao et al. (in press) reported similar findings when evaluating conventional loading against immediate loading protocols with mandibular two-implant overdentures in another systematic review and meta-analysis. In this paper, the number of implant failures reported was higher with immediate loading protocols, but the increase was not statistically significant.
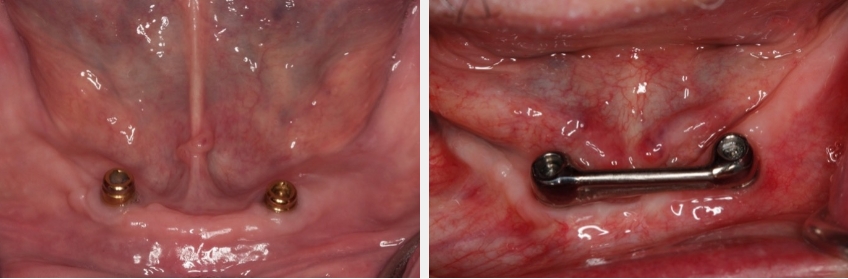
Neither of these papers reported on the influence of the prosthetic design of the mandibular overdentures utilized. Is there a difference in implant success or survival when a passive fitting tissue bar is used rather than resilient individual attachments, like locator or spherical attachments? An article from Elsyad et al. (2021) sheds light on this question by comparing overdentures with immediately loaded implants, “resilient stud” locator attachments, and a bar attachment. In this study, four implants were used in the mandible. At one year, the authors report implant survival as 96.6% for the locator and 98.3% for the passive fitting bar — no statistical difference.
These recent articles further support ITI consensus statements published by Gallucci et al. in 2014 regarding implant loading protocols for implant overdentures in edentulous jaws. According to this paper:
- “Current clinical research supports high survival using threaded, microtextured implants with a minimum diameter of 3.0 mm to support overdenture prostheses when used with immediate, early, or conventional loading protocols. Limited evidence exists for immediate loading of implants supporting overdentures in the maxilla.” 4
- “Descriptive material from the review in this group for immediate loading by Schimmel et al lists inclusion criteria of: insertion torque (≥ 30 Ncm), ISQ value (≥ 60), two or more implants in the mandible, or four or more implants in the maxilla.”4
- “Splinting of implants and the type of attachment system did not affect 1-year survival rate compared to freestanding implants.”4

The article then goes on to provide guidelines for clinical practice:
- “The intended loading protocol should be selected considering implant-prosthodontic parameters as well as functional, psychosocial, and financial aspects and patient preference.” 4
- “Early loading represents a satisfactory treatment modality in the management of the edentulous jaw, when using implants to support/retain an overdenture prosthesis and can be recommended as routine in the absence of modifying factors.” 4
- “Immediate loading protocols in implant-supported/ retained overdentures appear predictable. The available research arbitrarily uses an insertion torque of 30 Ncm or greater and/or an ISQ value of 60 or greater. The evidence for immediate implant loading in the maxilla is less compelling. However, there is no reliable pre-treatment predictor that has determined conclusively that the clinician can perform an immediate loading procedure.” 4
- “Given the lack of research, the use of a single implant in an immediately loaded fashion may not be indicated for support/retention of overdenture prostheses.” 4
In practice, I have found these clinical guidelines beneficial and a great conversation starter with our interdisciplinary team.
Conclusions and Final Thoughts
For overdentures in the mandible, immediate, early, and conventional loading protocols are all worth consideration.
The literature is unclear for overdentures in the maxilla, and conventional loading may be the most predictable approach. Other clinical variables, such as low insertion torque values or a patient’s history of bruxism, may alter the approach to implant loading with overdentures.
I hope you find the information helpful in treating your patients, and I look forward to hearing your thoughts about loading protocols and overdentures on Spear Talk and at your next visit to Spear Campus.
References
- Papaspyridakos, P., Chen, C. J., Chuang, S. K., & Weber, H. P. (2014). Implant loading protocols for edentulous patients with fixed prostheses: a systematic review and meta-analysis. International Journal of Oral & Maxillofacial Implants, 29.
- Borges, G. A., Costa, R. C., Nagay, B. E., Magno, M. B., Maia, L. C., Barao, V. A. R., & Mesquita, M. F. (2021). Long-term outcomes of different loading protocols for implant-supported mandibular overdentures: A systematic review and meta-analysis. The Journal of Prosthetic Dentistry, 125(5), 732-745.
- Cao, Z. L., Li, X., Lin, L. J., & Chen, Y. H. (2021). Immediate or delayed loading protocols for two-implant mandibular overdentures: A systematic review and meta-analysis of randomized controlled trials. The Journal of Prosthetic Dentistry, 126(6), 742-748.
- Elsyad, M. A., Alsabri, M. A., Elgamal, M., & Youssef Al-Tonbary, G. (2021). Resilient Stud Versus Bar Attachments for Immediately Loaded Implants Supporting Mandibular Overdentures: 1-year Randomized Controlled Clinical Trial. International Journal of Oral & Maxillofacial Implants, 36(2).
- Gallucci, G. O., Benic, G. I., Eckert, S. E., Papaspyridakos, P., Schimmel, M., Schrott, A., & Weber, H. P. (2014). Consensus statements and clinical recommendations for implant loading protocols. International Journal of Oral & Maxillofacial Implants, 29.
- Liu, W., Cai, H., Zhang, J., Wang, J., & Sui, L. (2021). Effects of immediate and delayed loading protocols on marginal bone loss around implants in unsplinted mandibular implant-retained overdentures: a systematic review and meta-analysis. BMC Oral Health, 21(1), 122.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Darin Dichter
Date: October 29, 2021
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


