Some Questions I’ve Been Asked About Occlusion Over the Years
I’ve been lucky enough to have had opportunities to give back and help others grow and understand dentistry. I’ve also been lucky enough to have had (and still have) great mentors who challenge me to keep me growing.
As a mentor to dentists in Philadelphia and for Spear and as an instructor of TMD and occlusal dysfunction at Temple University’s graduate ortho program, I’ve had to respond to many questions. Here are just a few.
How Do I Start Learning About Occlusion?
If you were like me, you left dental school very confused about occlusion. I attended several lectures and tried to incorporate what I learned — sometimes, what I did worked, and other times, it didn’t.
My journey to increase my understanding of function started when I took hands-on continuing education courses with mentors who would watch what I was doing and understand my thought processes. They would challenge me with questions that helped increase my understanding.
I was also lucky enough to have a mentor back home with whom I could share cases. His input especially helped during my early days.
If you want to start learning about occlusion, Dr. Frank Spear’s new occlusion pathway on Spear Online provides an updated pathway of occlusion CE courses. The “Evaluating and Treating Occlusion in the Clinical Practice” pathway consists of 11 comprehensive occlusion courses and one team meeting designed to help Spear Online members and their teams master occlusion core concepts.
I Did a Filling and Took It out of Occlusion, but My Patient Says It’s Still High. What’s Happening?
People tend to adapt to what they perceive as normal until the time comes when they don’t. Recognize that you are treating a patient and not just a tooth.
Now that the treated tooth is out of occlusion, your patient has new contacts that feel different. You’ll need to find a way to get the patient back to being comfortable.
Some dentists say, “It’s new and you will feel comfortable soon. Let’s check in two weeks.” But what is magical about two weeks? Wouldn’t it be better to know what the occlusion is like before you start treating?
Mark the area with articulating paper before you start. If you see lots of contacts all over the teeth, you may have just found a problem. Discuss the potential problem and your concerns with the patient before you start.
You only have to fall into this problem once or twice before you realize it’s good to evaluate occlusion before treatment. Often, the occlusion stress causes the tooth or the restoration to fail.
I like to document occlusion and discuss it with my patient early on. I mark with articulating paper during my photographic series before I take occlusal shots. Then, as I review the photos, I can share my concerns and explain to the patient how getting their bite right will help their dentistry last a long time.

My Patient Got Mad at Me for Grinding on Her ‘Good Tooth.’
If you go to a dental laboratory, you’ll see that most dentistry is single-tooth dentistry because it’s easy to sell a crown to someone who broke a tooth.
So, you tell your patient their tooth needs a crown, and the tooth dust flies! You take an impression and make a provisional restoration. Do your provisional restorations look beautiful? (A topic for a different article.)
Three weeks later, you start fitting the new crown. The contacts are good, it seats well, and the margins are closed. Life is good. Then you ask your patient to bite down and ask, “How does it feel?”
You spend 10-15 minutes grinding on the tooth to get it milled into occlusion. It now looks like a white blob. So, you think to yourself, “I have to change labs. They keep making the crowns too high.” Many dentists write on their lab orders, “out of occlusion.”
Then you realize the crown is getting too thin, so you grind on the opposing tooth. That’s when your patient stops you and says, “Why are you grinding on my good tooth?”

Is it a good idea to chat with your patient before you start? While your patient is getting numb, look at the opposing tooth. If there is a sharp or plunger cusp, let your patient know the opposing tooth may need adjustment to correct the results. If there is an uneven occlusal plane or uneven marginal ridges, chat with your patient about it.
This also may be a good opportunity to bring up the idea of looking at the rest of your patient’s occlusion to help prevent other teeth from failing.
Why Is Occlusion Important?
Occlusion isn’t necessary — except when it is. Since most dentistry is single-tooth care, most people adapt — except when they don’t. When they don’t adapt, problems occur.
“Everything was just fine until you put the filling in!”
As you learn and understand occlusion, you will start to see more. Please recognize that occlusion is not just about teeth. It’s a relationship between the teeth, muscles, and the TMJ, all functioning harmoniously. When one component is off, the other two will be affected.
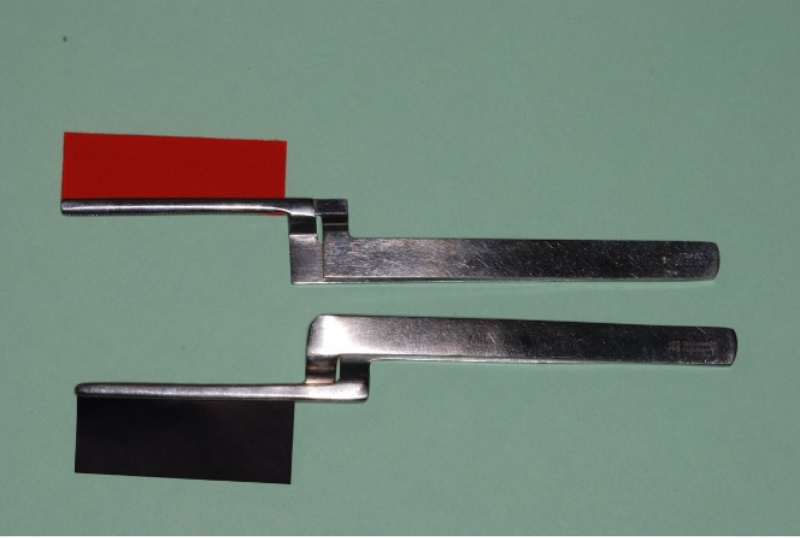
How do you evaluate tooth contact? Most dentists use articulating paper. When I ask, “What articulating paper do you use?” the most common answer I get is, “The one my assistant hands me.” Most dentists do not know the thickness of the paper they use. Most are too thick and will show marks that are not present.
As you understand occlusion and dentistry, you will start to look at the details. Your outcomes will become very predictable as a result. More questions and answers to follow. Good luck on your journey, may it lead you to where you want to go.
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Carl Steinberg
Date: November 20, 2020
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


