7 Steps to Using Retraction Cord When Making Impressions
One of the most challenging aspects of crown and bridge treatment is managing gingival tissue before making an impression.
The management includes placing the gingival tissues away from the prepared tooth margins so they can be impressed, combined with providing for hemostasis when the gingival tissues might bleed. Whether the impression is made conventionally with impression material or with a digital impression technique, all the tooth margins need to be captured to assure an excellent marginal fit of a lab-fabricated restoration.
There are many techniques to achieve retraction, including retraction cords, chemical reagents, electrosurgery, laser tissue sculpting, and hemostatic materials that displace tissue atraumatically. In most cases, gingival retraction cord is the most effective method. Controlling the soft tissue, managing any bleeding and exposing the margins is what’s most critical. That is why the clinician needs to understand all the choices available; one might choose a different alternative depending on the tooth being impressed.
Mechanical displacement of the gingival tissues aside from the tooth prep margins allow sus visualization and access, and we do this best with retraction cords. A survey of prosthodontists in 1999 showed that 98% of those who responded used retraction cord, and half of them used the double-cord technique. Back then, plain cord was the most commonly used cord, followed by aluminum chloride-impregnated cord.
Types of cords: Braided vs. knitted

Braided cords have a tight, consistent weave. For many clinicians, these are easier to place in the sulcus with packing instruments (serrated or nonserrated). Knitted cords unravel and fray less when cut during placement, so theoretically, they’re easier to place. Because they expand when wet, knitted cords will open the sulcus greater than the original diameter of the cord.
With either braided or knitted, there is a variety of diameters and sizes to allow for ease of placement in tighter and healthier gingival sulcuses. Ultimately, it is a personal preference.
One study showed that knitted cords were preferred over braided and there was no advantage to cords impregnated with epinephrine.1 It usually becomes a person’s preference as to what exactly is desired. Either way, when handling retraction cord, remember to use latex-free gloves because contamination of the cord with latex can have a deleterious effect on the setting of the VPS impression materials. This is important when a light-body material is placed first into the sulcus. If it doesn’t cure completely, it can result in inaccuracies or tearing of the fine gingival margin within the impression.
Cord packing instruments
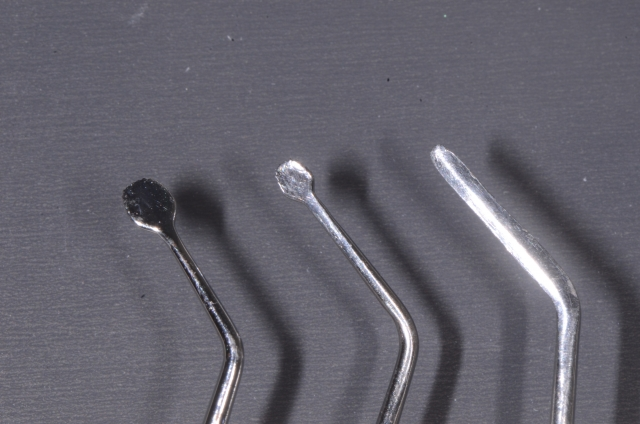
The end of the cord packer needs to be thin enough to be placed in the gingival sulcus without damaging the tissue and causing any bleeding. The angulation of the instrument will help in the orientation for the placement.
Many clinicians find that placing the cord with a nonserrated instrument is easier because the cord won’t pull back out of the sulcus. Design of the instrument varies by manufacturer, but many dentists use two different instruments depending on the tooth location — thin, flat instruments work quite well for anterior tissue (which tends to be thinner and tighter), and rounder, serrated or nonserrated instruments work better for posterior teeth.
Astringents and hemostatic agents
Astringents cause a contraction-retraction of the tissues, while hemostatic agents constrict blood flow through coagulation. These agents will initially cause a transient ischemia, shrinking the gingival tissue. These compounds include aluminum potassium sulfate, aluminum sulfate, 20–25% aluminum chloride, 15.5–20% ferric sulfate, and 4–8% racemic epinephrine.
Chemically impregnated cords offer better sulcus displacement because you have both a mechanical and chemical effect. When used for durations of less than 10 minutes, they cause minimal tissue damage. These chemicals can interfere with the surface detail of the impression material and with the dentin surface, so thoroughly cleaning the dentin before using a resin-bonded cement is recommended. (Click here for tips on choosing impression materials.)
Racemic epinephrine-impregnated cord can cause elevated heart rate and blood pressure (especially if placed into bleeding tissues), and literature shows there is no clinical benefit in gingival retraction with this. But if you still choose to use it, the 4% is safer for cardiac patients than 8%.2
One study examined the effect of presoaked cords on the microcirculation of the tissue at the gingival margin and found that blood perfusion fell markedly upon inserting the cord (with all the compounds). However, after five minutes the decrease became less apparent with cords impregnated with aluminum chloride and ferric sulfate. The epinephrine-soaked cord continued to affect blood flow for the next 20 minutes.3
The consensus seems to be that using presoaked cords is more convenient than cutting, soaking and blotting before placement. Remember, ease in placement process is desirable.
Finally it must be noted that these agents are acidic, ranging from 0.7 to 2.0 pH. They can remove the dentin smear layer and can cause postoperative sensitivity, so be sure to use a cleansing and desensitizing agent.
Cordless retraction
I’ve been a huge fan of cordless retraction products because they deflect tissue and control hemorrhage and moisture. It’s also much easier to syringe it in (less time and force) than pack cord in. If you have deep subgingival margins, these products don’t work as effectively.
I have used these products and find that they work pretty much the same. Expasyl, Traxodent, and GingiTrac are probably the most popular ones. They are made from a viscous paste of diatomaceous clay with aluminum chloride and require two minutes in the sulcus. They give excellent retraction that is nontraumatic and noninvasive. When used with a compression cap, they enhance the effects of the material. They can be used alone or with retraction cord.
How to use retraction cord
First of all, there is no “one size fits all.”
- Evaluate the health of the gingiva and the depth of the sulcus. Select a diameter that looks like it will fit. If there is minimal sulcus depth, it will accommodate only a single-cord technique, and probably only a thin cord. A deeper sulcus with healthy tissue accommodates a double-cord technique (thin in first, followed by a wider diameter). The initial, thinner cord controls any bleeding from the base of the sulcus. The cord works mechanically, but the astringent has the function of blocking sulcular secretion and hemorrhaging.
- Twist the first cord very tightly and loop it around the preparation. Overlap slightly and gently tuck it down beneath the shoulder of the prep. The cord will unwind a bit and force the tissue laterally away from the tooth.
- Next, twist the second cord tightly and repeat the process. Again, the cord will unwind slightly and force the tissue laterally.
- Leave the cords in place for 3–5 minutes.
- Right before making the impression, the cord should be wetted with water so it won’t grab and tear the tissues when it is removed, creating more bleeding.
- Once the cord is removed, the retraction is maintained for 30 seconds. Be prepared to begin immediate syringing of your impression material. If bleeding is persistent when the first cord is removed, go ahead and make the impression anyway, knowing it won’t be acceptable (don’t even look at it) but it will maintain retraction and give hemostasis. Once you remove it, immediately make a second impression because the sulcus will be open and not be bleeding. It does take more time and expense to do the double-cord technique, but many believe the accuracy of the impression makes it worthwhile.
- Some clinicians prefer to put the retraction cord in before finishing the preparation. Dragoo and Williams reported that this produced minimal gingival lesions and the best tissue results for operative procedures.
Cordless vs. conventional systems
When we compare cordless and conventional displacement systems, the results of one study showed that nonimpregnated displacement cord was the least effective in terms of bleeding and impression quality. So if you’re placing cord, use an astringent with it. Using a retraction cap with paste showed better results for ease of application, time spent, and bleeding management than aluminum chloride cord. Using both the aluminum chloride cord and paste-cap showed the best results for tissue management and impression accuracy, but was time-consuming and difficult. So except for the nonimpregnated cord group, all groups are comparable and clinically useful.
Ultimately, the most appropriate technique for the clinical situation is based on your comfort with your clinical skills, your knowledge, and your commitment to understanding that your choices will influence the accuracy of the impression and the response of the tissue.
When thinking about gingival retraction techniques, think about having a few options in your armamentarium to choose from. The tissue, the time and the ease of placement will probably determine how you will decide what you will do. All will work well if done well.
Lastly, who decides what cord to buy in your office? Is your purchasing assistant buying a “special” that you may never use or do they have no idea what the differences in the astringent agents are? How many cords do you really need and routinely use? Make sure you’re asking yourself these questions. It is worthwhile for all clinicians to review their protocol and understand all the choices available.
References
- Clinical trial of gingival retraction cords. J Prosthetic Dent. 1999 Mar; 8(3):258–61
- Human blood pressure and pulse rate response to racemic epinephrine retraction cord. J Prosth Dent. 1978 Mar; 39(3):287-92
- Effects of pre-soaked retraction cords on the microcirculation of the human gingival margin. Oper Dent. 2002 Jul–Aug; 27(4):343-8
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Mary Anne Salcetti
Date: November 16, 2015
Featured Digest articles
Insights and advice from Spear Faculty and industry experts



