Tracking and Controlling the Risk of Endocarditis With Dental Procedures
Every day, we encounter bacteria capable of inducing infective endocarditis, but for the most part, the risk is low. This condition has an annual incidence rate of about 3-10 per 100,000 people, but for that unfortunate few, it is life-threatening. While we can avoid risks in our daily lives, the dental office presents a different story. We must track and control the risk of endocarditis with dental procedures to protect our patients.

Assessing the risk of endocarditis with dental procedures
Infective endocarditis occurs when bacteria from the mouth enter the bloodstream, ultimately leading to life-threatening inflammation of the heart’s lining. While it can occur even without any invasive dental procedure, there are a few situations where the risk is heightened.
- Tooth extractions
- Periodontal surgery
- Implant placement
- Tooth replantation
Essentially, any procedures where the gums are manipulated extensively, or there is any perforation of them, could increase the risk that bacteria will make its way into the bloodstream. Of course, even if this happens, there’s no guarantee that the bacteria will affect the heart.
Some patients are at an increased risk of endocarditis with dental procedures due to preexisting conditions that affect their body’s ability to heal following surgery. We can categorize these into cardiac and non-cardiac diseases.
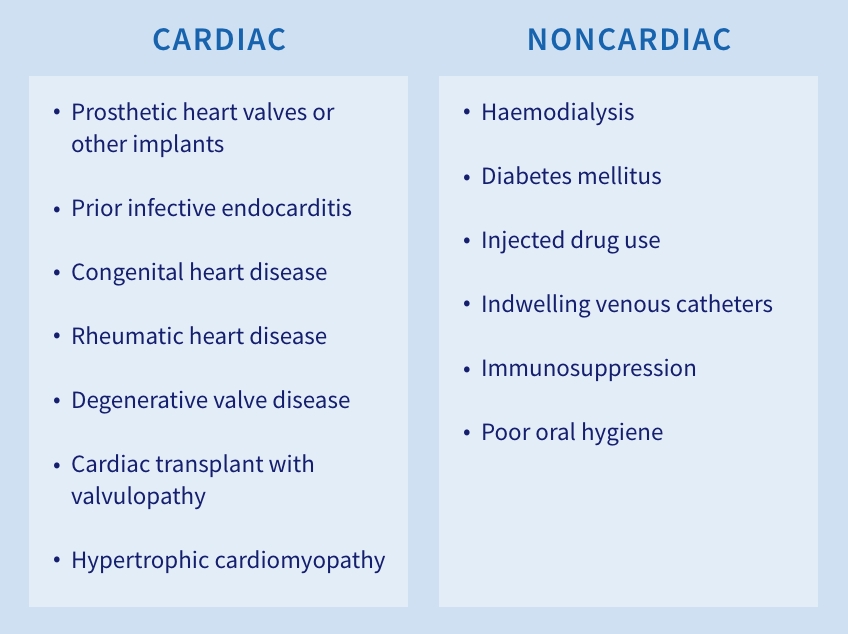
Most conditions are easy to assess as they’re self-reported. A patient reports prior cardiac surgeries or noncardiac conditions, which will trigger the need for a greater risk assessment, pre-treatment, and follow-up. What’s less clear is the risk related to poor oral hygiene. As some pre-treatment options for high-risk individuals carry their own dangers, it’s essential to assess this judiciously.
How to prepare and protect at-risk patients
The patient’s history and health conditions should trigger a risk assessment to weigh the need for invasive dental treatment against the risk of endocarditis. Educating patients, keeping track of their pre-and post-surgical condition, and providing preventive antibiotics can help you manage the risk of endocarditis with dental procedures.
Tracking and follow-up
Some studies have indicated that monitoring patients at moderate risk of endocarditis for four months following treatment can improve outcomes. Much of this center on how long it can take the condition to present following an invasive procedure. Some individuals did not report problems until nearly 120 days after procedures, for example, long after many dental offices would stop following up.
Monitoring may include regular phone calls, in-office check-ups, and even telemedicine reviews. Through patient tracking and follow-up, providers may be able to catch potential infections when small, before they trigger the need for in-patient treatment.
Antibiotic prophylaxis
In high-risk patients, antibiotics given before treatment can significantly reduce the risk of infective endocarditis. However, this is not recommended for all patients. Antibiotics carry their own risks, especially in patients with existing comorbidities.
To help address this, the American Dental Association and American Heart Association released guidance in 2007 on when pre-dental antibiotics may be advised and reinforced those standards after a review in 2021. Specifically, pre-surgical antibiotics are recommended when patients have:
- Prosthetic cardiac valves, or prosthetic material used in valve repair
- Prior infective endocarditis
- Prior cardiac transplants with valve involvement
- Unrepaired congenital heart defects including palliative shunts and conduits
- Some repaired congenital heart defects involving residual shunts or valvular regurgitation
This narrow window of patients ensures that they’re not put at risk unnecessarily while improving post-surgical outcomes.
Patient education
The American Heart Association has printed wallet cards for individuals at risk of infective endocarditis, complete with recommendations related to antibiotics. As endocarditis is a complex condition, it may be helpful to provide something like this to patients so they can better understand their condition and help others understand it as well.
When it comes to education, an ounce of prevention is worth a ton of cure. Educating patients on proper hygiene and follow-up care will be critical for reducing their risks. Clear explanations and regular preventative treatment can help them understand how to avoid this high-risk condition.
Prevention is key
Prevention is the key to controlling the risk of endocarditis with dental procedures. With regular follow up, appropriate preventative treatment, and patient education, offices improve outcomes and patient engagement.
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Spear Team
Date: December 22, 2022
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


