Management of Uncomplicated Crown Fractures in the Permanent Dentition
The loss of a tooth at an early age has a lifetime impact. Traumatic dental injuries, commonly known as TDIs, often occur in children and young adults, comprising 5% of all bodily injuries, according to a 2013 Journal of Endodontics article. The incidence is higher in U.S. school children, where 25% of them experience dental trauma. And the number of adults experiencing trauma to their permanent dentition is 33%, with most injuries occurring before age 19.
The etiology of TDIs is broad and includes behavioral factors, such as risk-taking children, obesity, amateur athletes, increased overjet with a protrusion, and other factors, like illness, learning difficulties, inappropriate use of teeth, or oral piercings.
Restorative dentists must be comfortable managing dental trauma cases such as uncomplicated crown fractures because proper diagnosis, treatment planning, and follow‐up are essential to ensure a favorable patient outcome. They must also be comfortable communicating treatment options and the prognosis to patients and/or a patient’s parents or legal guardians to obtain complete, informed consent for treatment.
Not accepting unscheduled emergency TDIs can be a missed business opportunity, considering the yearly treatment costs of oral injuries are estimated to be $2 million to $5 million per one million inhabitants. With crown fractures and luxation of the permanent dentition being the most common injuries, knowing how to manage these complex cases and feeling comfortable with the process can be a successful way to increase revenue for your practice.
Clinical Examination and Diagnostics of Uncomplicated Crown Fractures
Crown fractures are classified as:
- Enamel Infractions: A crack, or crazing, of the enamel without loss of tooth structure.
- Uncomplicated Crown Fracture (enamel only): A coronal fracture involving enamel only with the loss of tooth structure.
- Uncomplicated Crown Fracture (dentin and enamel): A coronal fracture confined to enamel and dentin without pulp exposure.
A clinical TDI examination should have good lighting and transillumination to evaluate teeth for fractures and infractions. Before testing for tooth percussion, a sensitivity assessment using air, usually done with a mouth mirror’s handle, should be performed.
To assess for a subluxation injury or root fracture, palpate the tooth and alveolus bi-manually. Tooth mobility is graded by applying pressure with the ends of two mouth mirrors (using fingers is unreliable since they are compressible) and attempting to move the tooth buccolingually.
According to the Grace and Smales Index, 1989, normal physiologic mobility is 0.25 mm, but an allowance should be made for pre-existing periodontal conditions. Mobility is graded as:
- Grade 0: no mobility
- Grade 1: mobility < 1.0 mm buccolingually
- Grade 2: mobility >1.0 mm but >2.0 mm
- Grade 3: mobility >2.0 mm or compressibility within the socket.
Determining the location of the fulcrum is also essential since teeth that are mobile at a point halfway along the root or less are likely to have a root fracture. Finally, assess for tooth vitality with electronic and thermal tests.
Without any clinical evidence of root fracture, a periapical radiograph using the paralleling technique is necessary. Film holders should be used to facilitate standardized and reproducible radiographs since the baseline image provides a reference for future comparisons at follow-up examinations. The recommended radiographs are:
- A periapical radiograph to demonstrate the two maxillary central incisors through the midline.
- Right and left periapical radiographs at the lateral incisors also show the canine and central incisors.
- A parallel periapical radiograph through the lower central incisors.
If the lost tooth fragment is not present, consideration should be given to imaging the soft tissues (e.g., the lips) to locate it.
Management of Uncomplicated Crown Fractures
Enamel Infraction
Usually, no treatment is needed except if the infraction is severe when etching and sealing with resin to prevent discoloration and bacterial contamination is considered. Does not require a follow-up.
Uncomplicated Crown Fracture (Enamel Only)
Treatment is dependent on whether the detached tooth fragment is available or not. If the fragment is available, it should be bonded back onto the tooth. Alternatively, depending on the location and magnitude of the fracture, a direct composite resin restoration can be placed, or the fractured edges smoothed with a disc. Follow-ups at 6-8 weeks and one year should be scheduled with a clinical examination and periapical radiographs.
Uncomplicated Crown Fracture (Enamel and Dentin)
If the detached fragment is available, it should be rebonded. Before rebonding, the fragment should be soaked for 20 minutes in a saline solution to rehydrate it. Alternatively, the tooth can be restored with direct composite resin or indirect ceramic, depending on the extent of the injury and the operator’s skill set. This procedure does not require a follow-up.
Case #1: Fragment Reattachment



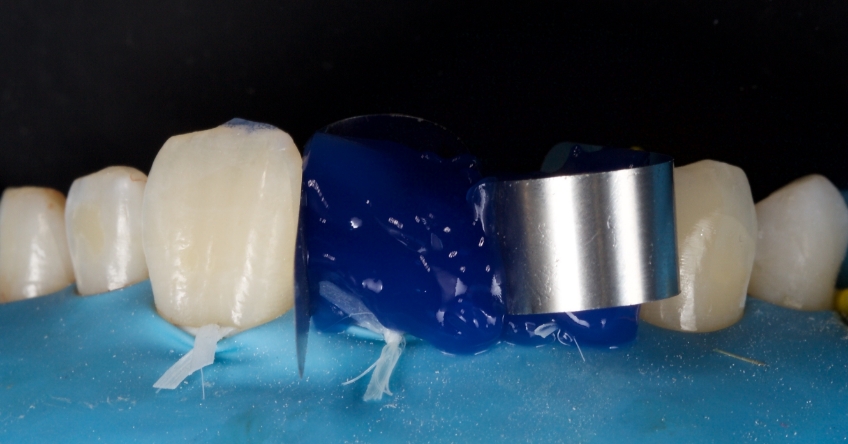
Any biofilm and aprismatic enamel were removed from the tooth, and the fragment was fragmented with light hydro abrasion with 29-micron alumina at 2-3 bar pressure. The tooth and the fragment were etched with 37% phosphoric acid (Ultradent), and a fourth-generation dentin bonding agent (Kerr, OptiBond FL) was applied (the adhesive component was not light-cured).
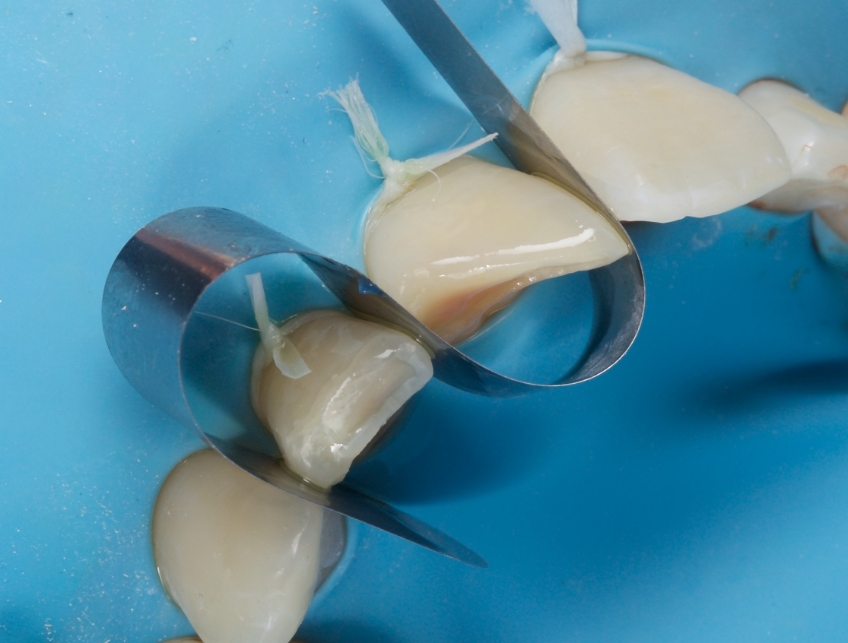
The fragment was luted to the tooth with heated chromatic enamel shade composite (GC G-aenial A2 shade). The heater used was a Calset Warmer from Addent. The excess composite was cleaned with an interproximal carver from American Eagle and smoothed with a number three brush and modeling resin (Brush & Sculpt from Cosmedent).
The composite was heated because it gained lower viscosity to improve adaptation. Plus, heating increases the conversion of monomer to polymer, which improves the physical characteristics of the resin, such as flexural strength and wear resistance, according to research by Da Costa, Hilton, and Swift in 2011.
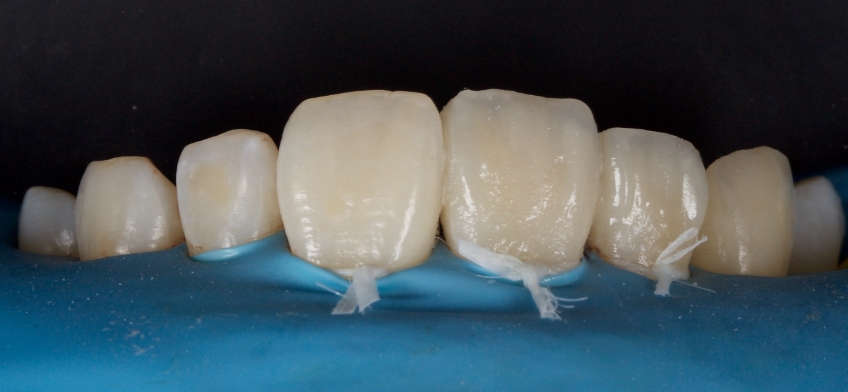
The resin was polymerized, and the oxygen-inhibited layer was removed by polymerization under glycerine.

The enamel fracture on 2.1 was untouched and will be managed in conjunction with esthetic management of the white hypo calcification at a later time.

Case #2: Restoration With Direct Composite Resin
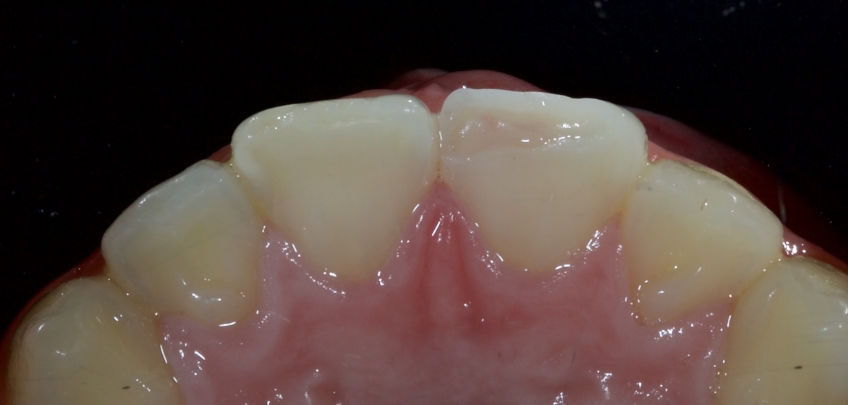
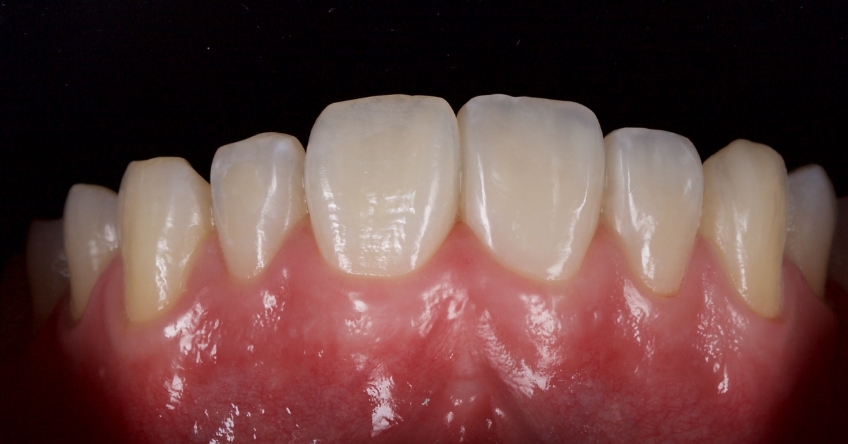
This 21-year-old male presented with an uncomplicated enamel-dentin fracture of the upper right central, lateral incisor, and canine following a fall.










Summary
A busy dental office must know how to manage uncomplicated crown fractures of permanent dentition efficiently and effectively. Reviewing case studies such as this and discussing complex cases with your peers is a great way to feel more comfortable and significantly impact the outcome for the patient.
References
- da Costa, J. B., Hilton, T. J., & SWIFT, JR, E. J. (2011). Preheating composites. Journal of Esthetic and Restorative Dentistry, 23(4), 269-275.
- Andersson, L. (2013). Epidemiology of traumatic dental injuries. Journal of Endodontics, 39(3), S2-S5.
- Glendor, U. L. F. (2009). Etiology and risk factors related to traumatic dental injuries–a review of the literature. Dental Traumatology, 25(1), 19-31.
- Sabuncuoglu, O. (2007). Traumatic dental injuries and attention‐deficit/hyperactivity disorder: is there a link?. Dental Traumatology, 23(3), 137-142.
- Moule, A., & Cohenca, N. (2016). Emergency assessment and treatment planning for traumatic dental injuries. Australian Dental Journal, 61, 21-38.
- Bourguignon, C., Cohenca, N., Lauridsen, E., Flores, M. T., O’Connell, A. C., Day, P. F., … & Levin, L. (2020). International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dental Traumatology, 36(4), 314-330.
- AM Grace, & FC Smales. (1989). Periodontal control: an effective system for diagnosis, selection, control and treatment planning in general practice. Quintessence Publishing Company.
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!

By: Jason Smithson
Date: July 19, 2022
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


