A Guide to Pre-Prep Diagnostic Mock-Ups
Esthetic restorative dentistry is at the heart of all restorative practices. The objective is to mimic nature with the beauty and contours of natural tooth structure. Our primary goal is to create an outcome that is not only esthetic but is both predictable and conservative with a treatment process designed to achieve a long-lasting restoration.
Studies indicate that the success rate of ceramic veneers’ 15-20-year survival is high, at 94-95%. With proper planning and preparation, a restorative dentist can also achieve outcomes at this high level of success.
The key to restoration success is to plan the cases comprehensively and develop a vision for the desired outcome. Using the concepts and processes from the workshop, Treatment Planning With Confidence, we can be more predictable regarding esthetic tooth position, functional contours, and management of structural integrity and biological health.
The Diagnostic Wax-Up
The diagnostic wax-up is typically used as a blueprint of the expected outcome. This wax-up visually references what changes may be necessary to achieve the desired result.
Diagnostic wax-ups are typically produced by the dental laboratory technician. Information for the treatment planning process is ideally forwarded to the technician through photographs, patient history, and FGTP templates. This information is transferred and incorporated into the wax-up.
Although the diagnostic wax-up represents the desired outcome, the preexisting tooth positions will affect what tooth contour changes will be necessary to achieve this result. The wax-up could be additive only, as in the case of retroclined or short teeth. Or the wax-up could be reductive, then additive, as in a case with proclined teeth that require a more palatal or lingual positioning to achieve improved esthetics and function.
The restorative clinician must know which type of diagnostic wax-up the technician created. This article will emphasize why, and more importantly, how the diagnostic wax-up changes are incorporated into the patient’s treatment process.
The diagnostic wax-up is a 3D rendering, generally created from 2D information. The photos and FGTP templates are very helpful in the waxing and contouring process. The final wax-up allows the restorative dentist to see the expected outcome in 3D.
The Mock-Up
As much as the dentist can interpret the changes made during the wax-up, it is very difficult for patients to perceive what effect these alterations will have intraorally. Most patients prefer to visualize ahead of time what the restorative changes will look like on their face and smile.
The standard tool for achieving this transfer of diagnostic information is an intraoral mock-up. Patient approval and treatment follow-through are more likely to occur following the diagnostic mock-up. Direct and indirect mock-ups may be utilized. Direct mock-ups are fabricated by applying composite resin intraorally on the patient’s teeth. The dentist can easily add tooth length or add tooth contours and then visualize them with the patient.
These mock-ups may provide instant feedback from the patient and help motivate the patient toward treatment. Direct composite mock-ups require variable chair time depending upon the number of teeth involved and the detail required to achieve the desired result.
Indirect mock-ups are generally more common but require more work and involve the dental laboratory-produced diagnostic wax-up. Once the wax-up is completed, a silicone or vacuum-formed matrix is fabricated. A self-curing provisional material, such as a bis-acryl, is loaded into the matrix and inserted over the patient’s teeth.
Once this material is cured or hardened, the matrix is removed, leaving behind bis-acryl with the exact contour and shape changes that were incorporated into the diagnostic wax-up. It is a beautiful duplicate of the exact changes that the patient can visualize in their mouth.
These mock-ups are used by dentists around the world to aid in educating patients, as tools to direct tooth preparation depth, and for evaluating proposed changes of tooth contour and shape.
However, there is a significant caveat to using these indirect mock-ups: They are only accurate if the wax-up was an addition. If the wax-up requires reduction or addition because of tooth position changes, then the teeth would require pre-preparation before placement of the indirect mock-up.
Although the literature is full of case studies that incorporate mock-ups as a routine part of a diagnostic work-up, there is very limited information and recommendation for pre-preparation recontouring before mock-up placement.
Accuracy is key when using mock-ups to guide tooth preparation and provisional placement when a reductive wax-up is utilized. The following case study will exemplify the use of a diagnostic mock-up and tooth pre-preparation.

Ron was referred to my office by my referring periodontist. Due to a history of tooth trauma, Ron experienced external resorption of the root of tooth #8. Due to the extent and position of the resorption, this tooth was removed. Since Ron was esthetically driven, he proceeded with orthodontics to improve his smile and tooth positions before replacing the missing incisor.
Following the orthodontics, Ron returned to the periodontist and had an implant placed at the tooth #8 position and was referred to my office following implant placement. I was not involved in the diagnostic or treatment planning process until this point. The concept of collaborative treatment planning is entirely another topic for another day. Regardless, I examined Ron and developed my treatment plan for restoring esthetics and function.
Ron presented with a desire to have brighter and longer incisors. Tooth #8 is a pontic wired to the lingual aspects of the adjacent teeth. Implant #8 is in the final healing stages. His comprehensive orthodontic treatment was complete, and he is ready to proceed with the restorative phase.
He has no medical issues, no tooth decay, and has had minimal restorative dentistry in the past. He presents with a relatively high smile line showing the gingival contours of the maxillary teeth.

The FGTP templates were applied to Ron’s photographs. Individual restoration of implant #8 would limit the esthetic outcome due to his high smile line and the uneven gingival contours. Following the application of the templates, it is recommended that both central incisors be restored to create a more esthetic outcome. The incisal edge of tooth #7 would be restored with composite following the definitive restoration of the central incisors. Ron agreed with this treatment plan.

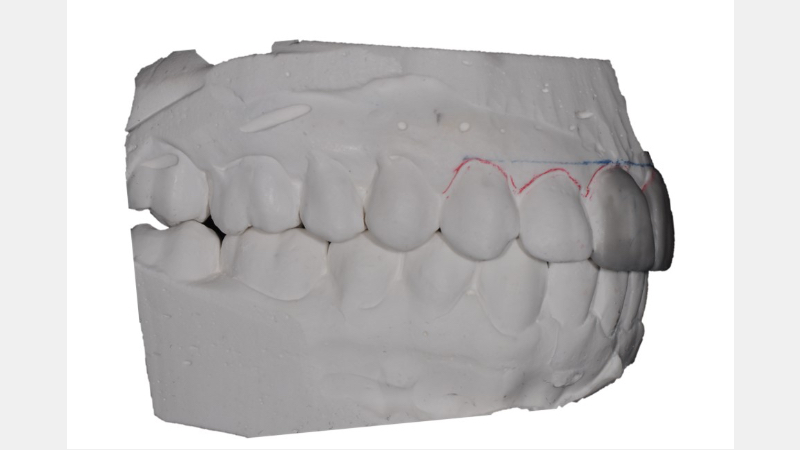
From the lateral aspect, the maxillary teeth are proclined relative to the occlusal plane. This tooth position results in shorter anterior tooth length. In addition to the unaesthetic tooth appearance, the functional requirement is also affected, and a reduction in the facial prominence of the anterior teeth is recommended.
The proposed treatment plan is to create a diagnostic wax-up incorporating teeth restoration #8 and #9. The wax-up will be reductive, then additive, to reduce the proclination of teeth #8 and #9. A mock-up will be applied as a reduction guide to minimize tooth over-reduction. The final restorations will be an implant post and crown for tooth #8 and an extensive veneer-lay for tooth #9.
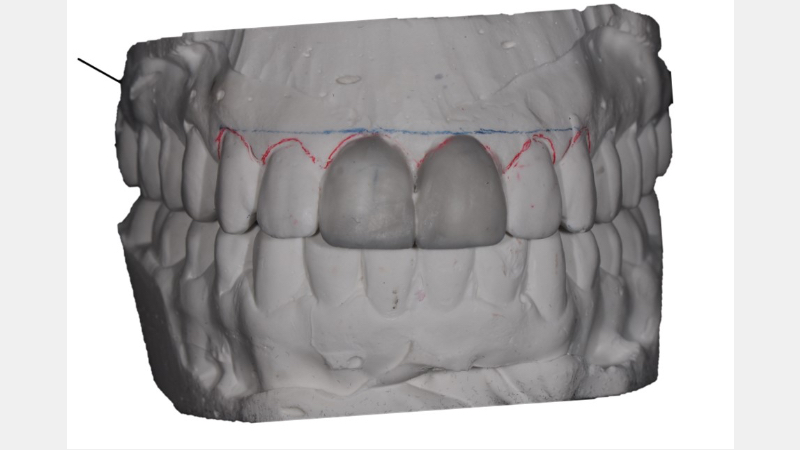
The diagnostic wax-up improves the overall tooth length and levels the gingival heights between teeth #8 and #9. It also reduces the facial proclination of the anterior central incisors. These contour changes result in a more ideal tooth proportion, enhancing esthetics and function.


Ron, like most patients, is a visual learner. It’s essential to allow patients to preview the proposed restorative changes before tooth reduction. As stated earlier, the diagnostic mock-up is a tremendous tool for allowing this preview opportunity. The accuracy of the mock-up is related to the precision of the outcome.
In Ron’s case, as in many other patients, there is a need for pre-recontouring of the proclined teeth to ensure the fit and accuracy of the diagnostic wax-up. Gurel refers to this process as aesthetic pre-recontouring (APR). The natural teeth must be trimmed or altered to allow passive seating and placement of the silicone matrix in the dental arch.
The silicone matrix is fabricated from the diagnostic wax-up and is termed a “window guide.” Once fabricated, it is removed from the wax-up model and trimmed to expose approximately 2-3 mm of the incisal edges of the anterior teeth.
The exposure of the edges allows the dentists to “view through the window” the accurate seating of the guide when placed over the teeth. Those teeth that interfere with the passive placement of the guide require alteration and adjustment. The technique of fabricating window guides is demonstrated in the Restorative Design workshop at Spear Education.

Ron declined the recommendation to place him back into orthodontics to correct the proclination of his anterior teeth. A window guide is necessary to correct the esthetics of the proclined teeth. The teeth’s facial positioning will not allow for the correct positioning of the diagnostic mock-up. By reducing the interferences before tooth preparation, the mock-up will accurately represent the final tooth contours created in the diagnostic wax-up.
Removing the interfering tooth structure (Fig. 9) allows for complete and accurate placement of the window index. In Ron’s case, the amount of tooth structure requiring removal was minimal, and no anesthetic was required. The diagnostic mock-up could then be placed appropriately and evaluated.

The mock-up is fabricated from a second index or matrix from the diagnostic wax-up. The matrix can be either a vacuum-formed clear “suck-down” material or silicone. Both can work if the accuracy of the fit can be verified. In Ron’s case, silicone was used for the matrix.
The matrix is trimmed in such a way as to minimize the overflow or excess bis-acryl. The facial gingival contours are removed, and the midline is marked as a reference guide. Complete and accurate placement of the silicone is key.

The diagnostic mock-up is placed and is now an accurate representation of the wax-up because of the pre-recontouring of the interfering tooth structure. The added tooth length may be visualized. The incisal edges and gingival contours are even. The mock-up may now guide the tooth preparations.

As discussed, Ron’s treatment plan called for extensive veneer-type tooth preparation. This preparation design and term come from the Restorative Design workshop techniques and concepts. The goal of Ron’s restorative treatment, and all other patient treatment, is to remain as conservative as possible and still achieve predictable esthetic and functional outcomes.
The extensive veneer creates adequate tooth reduction for material strength (EMax bonded restorations are planned) and shade change. The veneer preparation preceded the removal of the implant provisional, to better ensure precise margin placement, both facial and interproximal.
The window guide is placed on the final cast of the prepared natural central incisor. Complete seating of the index is seen with ideal facial and interproximal reduction.
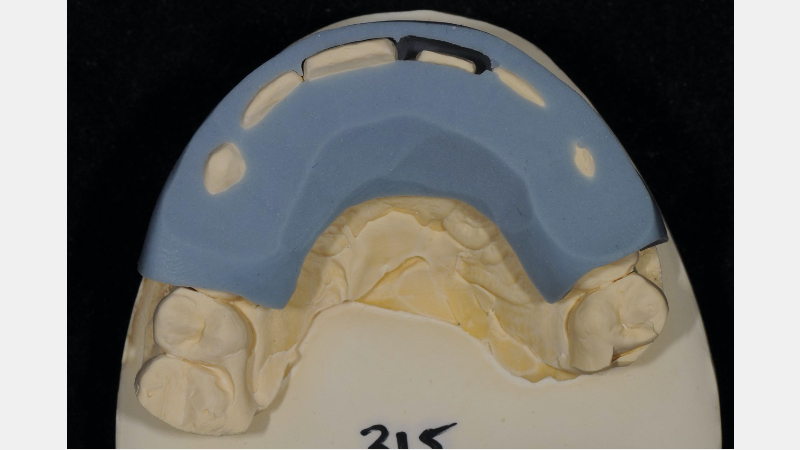
This ability to transfer the window guide with the same accuracy verifies the importance of pre-preparation recontouring of teeth. Ron’s case is nearing completion, but incorporating a window guide for pre-recontouring interfering teeth is key to its success.
The predictability of esthetic restoration is magnified by incorporating this technique into the restorative dentistry we perform. See a brief list of literature citing the concept of mock-ups and pre-recontouring for accuracy below.
Literature Review
This article discusses pre-prep reduction of teeth using vacuum templates fabricated from diagnostic wax-ups.
- Çötert, H. S. (2016). Reducing oversized tooth dimensions by using porcelain laminate veneers designed by diagnostic additive wax-up and indirect resin composite mock up. Madridge Journal of Dentistry and Oral Surgery, 1(1), 13-8.
This is a case study on mock-ups fabricated by increasing tooth volume for veneers and using silicone templates to fabricate mock-ups and preparation guides.
- Coachman, C., Gurel, G., Calamita, M., Morimoto, S., Paolucci, B., & Sesma, N. (2014). The influence of tooth color on preparation design for laminate veneers from a minimally invasive perspective: Case report. International Journal of Periodontics & Restorative Dentistry, 34(4).
This article reviews the importance of the diagnostic phase, diagnostic wax-up and dental lab communications. The diagnostic approach section discusses the need to modify tooth structure by reducing contours (subtraction) prior to mock-up application.
- Magne, P., Magne, M., & Belser, U. (1993). Natural and restorative oral esthetics part I: rationale and basic strategies for successful esthetic rehabilitations. Journal of Esthetic and Restorative Dentistry, 5(4), 161-173.
This article provides information on tooth preparation guides and technique.
- Brunton, P. A., Aminian, A., & Wilson, N. H. F. (2000). Tooth preparation techniques for porcelain laminate veneers. British Dental Journal, 189(5), 260-262.
Fig. 9 in this article addresses the requirement to pre-prep teeth to allow proper seating of the silicone index made from the diagnostic wax-up.
- Gürel, G. (2007). Porcelain laminate veneers: minimal tooth preparation by design. Dental Clinics of North America, 51(2), 419-431.
This article is a more complete version of the above article with same photos and discussions about pre-recontouring teeth but includes photos of reduction burs (all three bands of the same dimension).
- Gürel, G. (2003). Predictable and precise tooth preparation techniques for porcelain laminate veneers in complex cases. International Dentistry South Africa, 9(1), 30-40.
This article shows good images and describes (in Italian) the need for pre-recontouring of crowded teeth prior to placement of the diagnostic wax-up and provisionalization.
- Fichera, G., Sacco, G., Dinapoli, C., & Re, D. (2007). Restauri estetico-adesivi indiretti nei settori anteriori.
Study showing 94-95% survival of ceramic veneers after 15- years.
- Friedman, M. J. (1998). A 15-year review of porcelain veneer failure–a clinician’s observations. Compendium of Continuing Education in Dentistry (Jamesburg, NJ: 1995), 19(6), 625-8.
This article discusses a 20-year follow-up/survival ceramic veneers 94-95%.
- Calamia, J. R. (2004). Etched porcelain laminate restorations: a 20 year retrospective. Part, 1, 137-145.
VIRTUAL SEMINARS
The Campus CE Experience
– Online, Anywhere
Spear Virtual Seminars give you versatility to refine your clinical skills following the same lessons that you would at the Spear Campus in Scottsdale — but from anywhere, as a safe online alternative to large-attendance campus events. Ask an advisor how your practice can take advantage of this new CE option.

By: Jeffrey Bonk
Date: October 9, 2020
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


