How Dentist-Laboratory Relations Are Changing in the Digital Age
By Edward Roman on January 16, 2019 | 6 commentsIn the not-so-distant past, our knowledge of what we knew about lab work was based on wax, plaster, and centrifugal casting machines. As dentists, this was our world. We could grasp these concepts and essentially understood what was happening in the lab. Our prescriptions were, essentially, “PFM A2.” We would stick it in the box with the impression and, lo and behold, a cast coping with some feldspar baked on it would come back to us in a week or two. My, how things have changed!
Let’s take a journey to see how the relationship between our beloved and trusted labs has changed and created a whole new thought process with how our cases are communicated, prescribed and fulfilled by the dental laboratory.

The Prescription
As discussed previously, the prescriptions were rather simple. Carbon paper or NCR (no carbon required) were the extent of the lab slip. The dental office would take the impression, send a bite with an opposing model and (hopefully) the shade that they selected. The case was put in a box where it was either mailed using US Postal Service or, if geography permitted, picked up by your friendly local dental laboratory.
Now, there is so much more information that can be submitted in a more expeditious manner. Most labs now have a portal link to their website where the dental office can upload digital data along with the usual prescription information to aid the laboratory during the fabrication process. This protocol allows dentists to provide more detailed prescriptions to the lab, where it is immediately received through your favorite communication device. This helps the lab prepare for the case before it arrives physically on-site or before the scan file is transmitted.

Digital Communication Software
Several years ago, at a Quintessence Ceramics Symposium, I attended a lecture given by the esteemed Galip Gurel of Istanbul, Turkey. The dental laboratory of Dr. Christian Coachman from Sao Paolo, Brazil received the digital information from Dr. Gurel and completed the case in one day with overnight shipping to Dr. Gurel's office for delivery. This is when I knew that the dentist-laboratory relationship was forever changed.
Dental laboratories operate and maintain different types of communication software for different applications. Labs need to have multiple design systems for implant planning available to their clients and be proficient with those systems. This is where we overlay our digital restorative design with the DICOM (Digital Imaging and Communication in Medicine) file from the CT (computerized tomographic) file.
For restorative treatment planning, we use Team Viewer and Go To Meeting so the dentist can collaborate with the lab planning in real time instead of shuffling models back and forth between the dental office and the lab. Communication software gives the dentist the ability to review cases in three dimensions during the lab communication process. Visualizing the case allows the dentist and lab to learn together and quickly obtain a solution for the patient.
This asset has become a valuable time-saver for dentists adept at using this tool, and leads to an increase in their productivity. Less time chasing physical model treatment planning translates to more time treating patients.

Lost Wax
Stone models prepared in order to accept a physical wax design have rapidly given way to digital restorative design.
Wax has not completely melted away, though. It is still used for minor touch-up of stone models in our lab and our dental office. In no way will it ever return to its previous diagnostic prowess because of the efficiency and power of comprehensive digital design using programs such as 3Shape, Dental Wings, Exocad and CEREC design software.
Changing marginal ridges, line angles, occlusion and incisal edges is more quickly, efficiently and accurately performed using a mouse instead of wax instruments. Designs can then be 3D-printed in the lab or digitally returned to the dental office for fabrication on their own 3D printer. 3D models are more durable if transporting, since wax is fragile and has a tendency to chip if not gently handled.
Smile Design
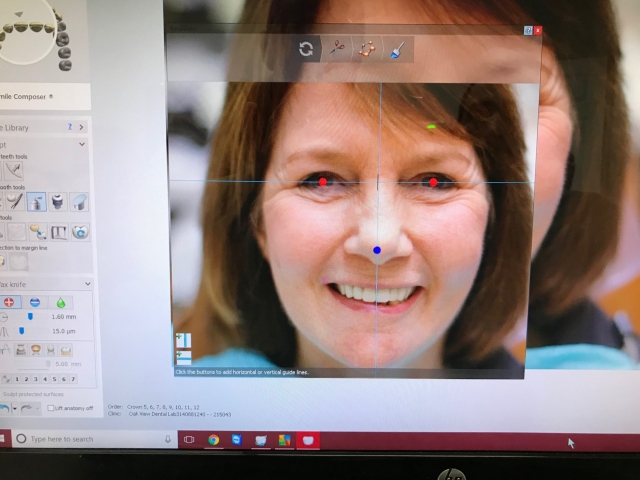
“The face is where it’s at” has become the mantra for smile design. The foundation of EFSB (Esthetics, Function, Structure, Biology) is to use the whole face to decide where the teeth optimally fit into the whole scheme of the treatment plan. Our lab receives digital files from the dentist hopefully including a full complement of photographs as described in EFSB.
Once the digital restorative design is completed using CR mounted casts as a reference, we introduce and align the digitized face image into the proposed restorative design. We then can preview the smile, evaluating our restorative design as it is proposed, using the face as our reference. These results are then sent back to the dental office for their evaluation and to share with a patient who has now become excited about the whole process. We have found that using this process allows the dentist and patient to come to a mutually acceptable solution to their objectives and confidently proceed with treatment.

Shade Taking
In the not-so-distant past, it was easy for labs and dentists to communicate shades, since the standard of care in the esthetic zone was the PFM (porcelain fused to metal). Now dentists and labs do not only have to address the various ceramic materials, but also heightened patient esthetic awareness. Now we have full-contour zirconia, layered zirconia, high translucency zirconia, layered and full contoured lithium disilicate and full contour leucite from which to choose the best solution for our patient.
High-resolution digital photography is used to obtain information using the various shade systems to communicate hue, value, chroma and surface texture. Dentin photographs and dentin shade guides are vital to success for any ceramic case.
The translucency never needed to be communicated with PFMs, since there was none. Now, important information on translucency needs to be provided prior to fabrication using photography. This will allow your lab to assist you in deciding which material best suits your patient's need. As dentists, we have all encountered the dreaded “shadow” after cementation due to us not communicating and addressing dark dentin and a high translucent ceramic. This can easily be prevented now with digital communication of our choice of ceramic in conjunction with an accurate dentin shade. Digital shade communication devices can also be used to transmit even more nuanced esthetic information to the laboratory.

Occlusion
Extensive occlusal adjustment for our laboratory’s dental clients regarding single unit restorations has essentially become a thing of the past for our dental clients. Dentists today are much more aware of productivity issues. None of our clients enjoy taking 30 minutes from their day to insert a single unit sent from their lab.
In our laboratory, we discuss specific parameters and restorative requirements for each of our clients. We then establish a file that is used to incorporate the dentist’s preference into each of their prescriptions. Contact tension, marginal ridges, force of occlusal contact and emergence profiles can then be consistently duplicated for each prescription using digital archiving, allowing for a much more predictable insertion experience.
Communicating occlusal requirements for the more comprehensive restorative cases is a more methodical and detailed process requiring several more layers of decision-making in occlusal design. Articulated casts or printed models are mounted on an articulator in centric relation. Once again, using EFSB principles, a restorative solution can be proposed using the digital design process.
In the past, this would involve sending gypsum models on the dentist’s articulator to the lab (unless the lab happened to have the same articulator calibrated to the dentist’s articulator) for a physical wax-up, which would then need to be sent back to the dental office for evaluation. If any changes were needed, the whole process of back and forth would be done again until there is an accepted design. This process had an inherent tendency to inhibit productivity and would invariably lead to unnecessarily long treatment times.
With the advent of the virtual articulator, the design process can be distilled down to a few steps done remotely in a matter of hours. The digital design is done as previously described using the EFSB process, but now the design can be integrated into the virtual articulator. All the design software systems we use in our lab now have several choices of articulators. We can now verify jaw movements to refine excursions, plane of occlusion, envelope of function and any other movement the dentist requires. With the newest scanners, our lab can actually place the whole articulator inside the scanner and duplicate the existing occlusion. From there, the restorative design can be completed with data extrapolated from the articulator.
Implant Planning
The first implant I restored was a Steri-Oss implant in 1986. The surgeon did an excellent job of placing it and I am pleased to report that it is still functioning well. However, I am fortunate that the implant was well-integrated and well-placed to function in an overall restorative scheme. My prescription referral was nothing more than “implant in the area of #13.” Computed tomography scans (CTs) were not done because they did not exist for dental implant applications (to my knowledge).
Now, the standard of care paradigm has dentists and labs requiring a CT, a digital restorative design overlaid with the DICOM file from the CT and (typically) a printed surgical guide to facilitate optimum placement prior to any treatment. What happens when the implant is not placed in an optimum restorative position is that our lab has to discuss other, more complicated and less-than-ideal solutions. When the validated workflow that we described above is used, predictability reigns and everyone is happy, especially our beloved patient.
The Test Drive
In the past, the lab slips we received would say “Crowns on #s 6-11, shade A1”. Most of the interpretation would be left to the lab tech. When the tech would call the dentist with questions about length, occlusion, incisal embrasures and other parameters, the dentist would many times say, “Uh, just do the best you can.”
Thankfully, our lab does not see this much anymore, especially with Spear dentists faithfully implementing EFSB principles. However, even with this process, there may be questions about how the case really looks in the mouth before it is started, even with meticulous treatment planning.
Now we are able to do additive digital designs, print a model of the design, make a copyplast template and send it to the dentist for a bisacryl mockup so the dentist and patient can preview the smile for length, height-to-width ratios, gingival profiles, color and any other diagnostic information that is important to the patient and the dentist. This allows the patient to have additional input for the dentist and the lab when the patient accepts treatment. The question of “how will it look when it is done?” can now be definitively answered.
We are also seeing a trend with clinicians using individually-milled PMMA (polymethyl methacrylate) provisionals based on the final scan/impression. The lab designs and fabricates individual PMMA provisionals that are based on the final restorative design. They are inserted and evaluated for final fabrication using our traditional provisional process. This adds a more detailed ability to make easily-communicated decisions on their esthetic properties before the case is prepared in ceramics. Once everyone is happy, the final case is precisely milled in ceramic using information derived from the PMMA provisionals.
Tissue development for implants in the esthetic zone can be a time-consuming process in the dental chair with temporary implant abutments, templates and trimming with polishing. Now, chair time can be reduced and productivity increased considerably by scanning or taking a physical impression of the implant on the day of placement (if primary stability is acceptable) and sending it to the lab for digital fabrication. Clinically, this takes a lot less chair time than hand fabrication.
The lab then returns an implant provisional the same day or the next day (usually milled PMMA) and the provisional is inserted with minimal chair time. In this way, the patient and dentist can visualize the desired result and make changes accordingly by simply communicating the changes to the lab. There is no need for further impressions since the digital file already exists.
The lab easily makes changes and sends another provisional back to the dental office for quick delivery and insertion. This technique can easily be repeated until the tissue emergence, form, shade and esthetic concerns are acceptable to the patient. Once the implant is integrated, the provisional can be converted to the ceramic of choice, leading to a highly predictable final restoration.
The Future
The only thing that can currently be predicted in dental laboratory technology is the fact that change is occurring exponentially. We are seeing trends away from milling machines and more towards printing.
Of course, milling machines will still be a standard of fabrication in the near future. However, once 3D printers begin offering a greater choice of materials (especially ceramic printing) and showing a reduction of capital costs for these machines, you will see an increase in their prevalence, especially in dental offices.
Communication technology is another area that has made significant leaps of achievement recently. We can now communicate over great distances with large volumes of information that allow the dentist to choose from a network of dental lab professionals that offer the best solutions for any particular case.
However, we must never lose sight of the most important relationships that will never change: our relationship with our patients and with the labs who provide faithful service to their clients. Technology is simply a vehicle that helps us build those indelible bonds of trust with your patients and with the professionals that help you achieve success.
Dr. Edward Roman, D.D.S. https://www.romanvaughan.com/
Comments
January 18th, 2019
January 18th, 2019
January 18th, 2019
January 18th, 2019
March 24th, 2019
March 24th, 2019