Horizontal Root Fracture: Extract or Retain?
Imagine if this were your new patient:

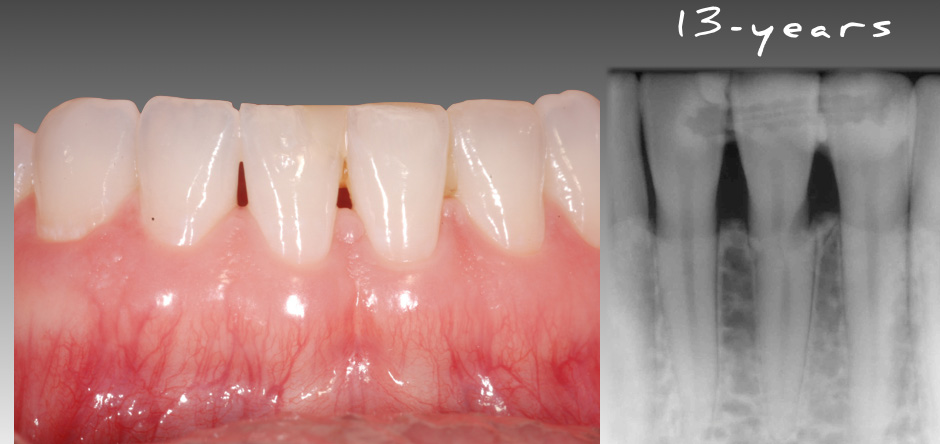
The tooth had been traumatically fractured and bonded back in place with a Ribbond composite splint. The tooth is asymptomatic when you see the patient. What would you do? Would the discussion revolve around extraction and implant placement utilizing a small diameter implant or a resin-bonded bridge? Or would you leave the tooth and monitor the patient over time? How predictable is a tooth like this in the long term?
It’s not uncommon for a tooth like this to be extracted from looking at and treating the radiographic appearance. However, if we look at the dental literature on the prognosis of horizontal root fractures, we may decide that the tooth should be retained.
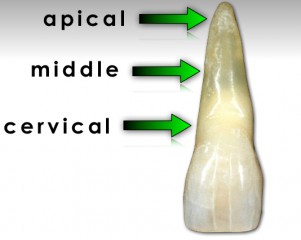
Andreasen and his group did a great piece of dental literature: They looked at the survival of 534 incisors after intraalveolar root fracture in patients ages 7–17. The paper classified the fracture location as cervical, cervical-middle, middle, or apical one-third (Fig. 1). It was found that 78% of the teeth showed healing of the fracture (either by hard tissue, fibrous, or osseous), with no difference between fracture positions on the root.
In 85% of the teeth, this healing remained unchanged throughout the control period, with no posthealing complications. At 10 years, there was an 80% survival rate. The highest frequency of tooth loss (70%) was with teeth that had cervical fracture locations. If you removed the teeth with cervical fracture locations, the 10-year success rate rose to 88%.
So when you look at the literature, teeth have a high degree of long-term success with horizontal fractures as long as the fracture isn’t located in the cervical third. This finding makes sense if you consider that the nearer the fracture is to the osseous crest, the less root is present in bone to support the tooth crown.
Looking at the image below, we can see that the fractured central incisor is still functional and serviceable at 13 years old. Although this case is not the norm (because of the long-term success despite the location of the fracture being in the cervical third), hopefully it makes you stop and think differently about managing teeth with horizontal root fractures.
Reference
Cvek, M., Tsilingaridis, G., & Andreasen, J. O. (2008). Survival of 534 incisors after intra‐alveolar root fracture in patients aged 7–17 years. Dental Traumatology, 24(4), 379-387.
FOUNDATIONS MEMBERSHIP
New Dentist?
This Program Is Just for You!
Spear’s Foundations membership is specifically for dentists in their first 0–5 years of practice. For less than you charge for one crown, get a full year of training that applies to your daily work, including guidance from trusted faculty and support from a community of peers — all for only $599 a year.

By: Greggory Kinzer
Date: August 24, 2017
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


