Ankylosis Part II: Treating Adults With an Ankylosed Tooth

Several factors need to be taken into consideration when deciding on the appropriate treatment option for an ankylosed tooth. These factors include:
- Whether the ankylosed tooth is deciduous or permanent
- The time/age of the onset of ankylosis
- The time/age at diagnosis
- Patient gender
- The location of the affected tooth
- The patient’s smile line.
The root of the ankylosed tooth will typically undergo continual resorption and subsequent replacement with bone. In addition, depending on when the tooth ankylosed, a hard/soft tissue defect in the area of the ankylosed tooth will be present if the tooth became ankylosed before completion of growth and development.
If, however, the tooth became ankylosed after growth was complete, there may be no impact on the hard and soft tissue positions. The patient in Figure 1 is in her late 50s and has tooth #9 ankylosed. Given the position of the gingival margin and incisal edge of this tooth compared with other teeth in the arch, it is apparent that it became an ankylosed tooth at some time prior to the completion of growth.
In contrast, the patient in Figure 2 is his mid-30s and also has tooth #9 ankylosed, but the gingival margin is level with the adjacent central incisor, leading us to conclude that it became an ankylosed tooth after growth was completed.

Treatment planning
When treatment planning an ankylosed tooth in an adult, it must be stated that the ankylosed tooth does not need to be extracted just because it is ankylosed. If you think about it, an ankylosed tooth is not that dissimilar from an osseointegrated implant. The treatment decision on whether to keep the ankylosed tooth — and possibly restore it — or remove it will depend on the esthetic impact of any hard/soft tissue defect and the rate at which the resorption is occurring.
If the treatment chosen is to keep the ankylosed tooth, many options exist:
- Keep the tooth and restore in its current position
- Subluxate the tooth and orthodontically reposition into the desired location
- Move the ankylosed tooth into the correct position using a segmental osteotomy containing the ankylosed tooth.
If the patient has a low smile line — or the gingival margin position is still correct and the rate of resorption is slow — keeping and restoring the ankylosed tooth in its current position is a simple way to improve the esthetics. The unknown of this treatment option, though, is how long the tooth will last before the resorption advances to the point the tooth structurally needs to be extracted. Even though there is a significant gingival margin discrepancy on the ankylosed tooth #9, the impact on the overall esthetics is low because of the patient’s low smile. (Figure 3)

Given that the resorption is occurring at slow rate — the tooth became ankylosed before the completion of growth and the patient is now in her late 50s — the treatment plan was just to restore the incisal edges of #8, #9 and #10 with composite. The composite restorations were in place approximately 10 years before the resorption advanced to the point that #9 required extraction (Figure 4).

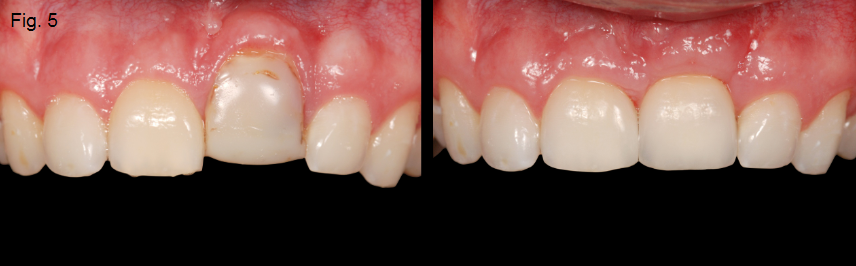
If the ankylosed tooth is an esthetic issue and the rate of the resorption is advancing quickly, extraction of the tooth is recommended. The area will typically require augmentation with either hard or soft tissue, depending if the final restoration is a single-tooth implant or a tooth-supported FPD (Figures 5 and 6).

(Read Part I of this series covering etiologies and considerations for ankylosis.)
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!

By: Greggory Kinzer
Date: October 6, 2016
Featured Digest articles
Insights and advice from Spear Faculty and industry experts



