Implants vs. FPDs for Single Anterior Tooth Replacement
It’s essential to identify what variables need to be evaluated in making a decision, recognizing that there will be times when either choice is acceptable.
When evaluating different treatment modalities, it’s helpful to break the assessment into the same categories used in the Facially Generated Treatment Planning process: Esthetics, Function, Structure, and Biology.
Esthetics deals with fundamental issues such as tooth position, gingival levels, papilla levels, tooth arrangement, contour, and color.
Function assesses joint issues, muscle issues, occlusal relationships, tooth wear, mobility, fractures, and the search for an occlusal etiology.
Structure refers to how we restore or replace teeth and understand the existing condition of all teeth, which teeth need restorations or replacement, and what options exist for the restoration or replacement.
Biology assesses all soft tissues, including the gingiva, for health or disease, and the treatment options necessary to correct soft-tissue problems. The same is done for bone.
All of these categories must be evaluated when deciding between single-tooth implants and fixed partial dentures (FPD).
Although I will list each category in a specific order, the key is to evaluate each point, not necessarily follow the exact order. Soft tissue and osseous requirements for an acceptable single-tooth implant are more demanding than an FPD, so I usually start my decision-making process with a biologic assessment.
Biology — Facial Bone
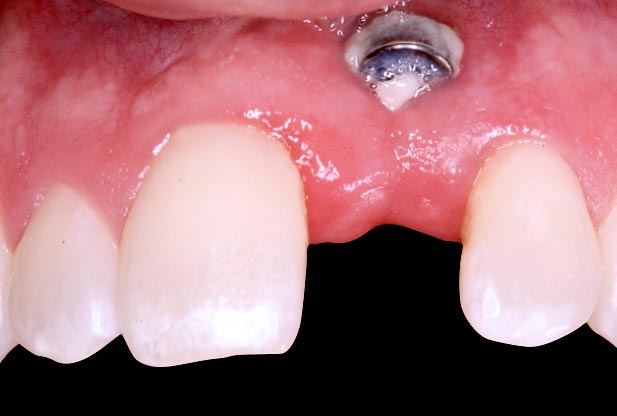
Is the available facial bone adequate in width and height for implant placement? If not, is augmentation a realistic possibility? If augmentation is possible, will the patient be willing to undergo the necessary surgeries? An FPD is the best treatment if not (Fig. 1).

While a single tooth posterior molar implant can be acceptable if there is adequate bone for placement and integration, there are much greater demands for an esthetically excellent single anterior implant. In fact, significant facial recession is one potential complication of a single tooth anterior implant when the facial bone and soft tissue thickness is not adequate1.
Biology — Interproximal Bone on Teeth Adjacent to the Potential Implant
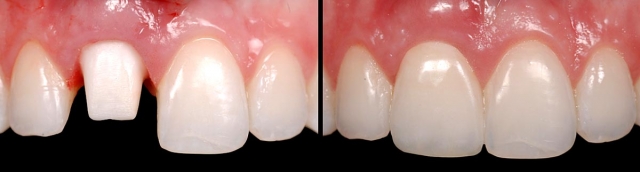
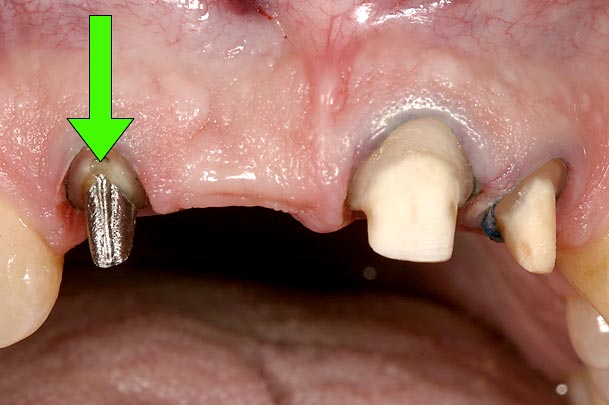
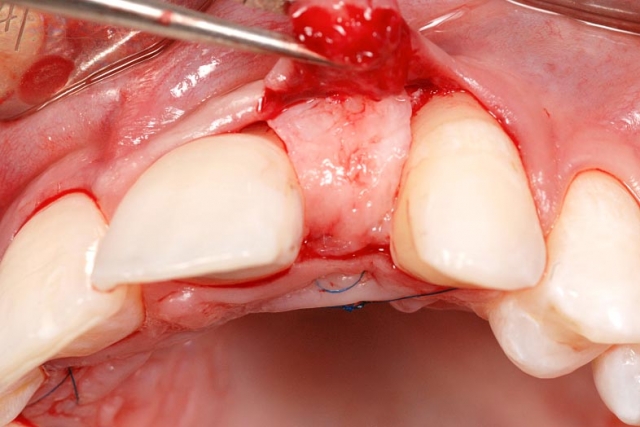
An esthetically excellent single-tooth anterior implant depends upon the interproximal bone on the adjacent teeth for its papilla height and on the facial bone level and soft-tissue thickness for a pleasing gingival margin.
Research reports an average papilla height of 4.5 mm above the bone on the adjacent teeth as a predictable papilla level following implant treatment.2 This means if there is interproximal bone loss on the adjacent teeth, the papilla between the teeth and the implant may be esthetically unacceptable.
In this case, an ideal result will require the adjacent teeth’s orthodontic eruption to move the interproximal bone to a more coronal position. The eruption may result in the adjacent teeth needing subsequent facial crown lengthening and restoration (Figs. 2–4).



In these cases a connective tissue graft and FPD, or an FPD using pink ceramic or composite to replace the inadequate papilla height may be a more predictable esthetic option than the compromised single tooth implant unless the patient considers the orthodontic eruption.
Biology — Space for the Implant
Assess the space for the implant, specifically between the contacts of the adjacent teeth, at the crest of the bone, and between the roots near the apex. Maxillary laterals and mandibular incisors are the most difficult teeth to manage for adequate space, but with modern 3.0-3.3 mm implants, a space of 5.0 -5.5 mm is typically adequate for placement.
If adequate space doesn’t exist, orthodontics will be necessary to create it, or else an FPD is indicated (Fig. 5).

Biology — Age and Facial Growth
We know that if an implant is placed, it will not erupt over time like natural teeth. For this reason, especially on single anterior implants, facial growth must be complete prior to implant placement. If not, as vertical facial growth continues, the teeth will erupt, and the implant will appear to intrude (Fig. 6).
There is no specific age at which everyone stops growing, but rather a range of ages. My team has traditionally used serial cephalometric radiographs done one year apart to monitor facial growth. If the two radiographs were identical, we would consider implant placement. If the newer radiograph shows vertical facial growth, we would wait a year and do another radiograph.
There are also large differences between when growth stops for females and males3. We would do the first radiograph in a female around age 17 or 18, but in a male, not until age 20 or 21.
If growth is not complete, a conservative bonded FPD is an excellent interim restoration until growth is complete (Figs. 7–10).



Biology — Pulp Size in Young Patients
The size of the pulp is an issue when replacing single anterior teeth in young patients. If the pulp is extremely large, a conservative bonded FPD is an excellent alternative to prepping a tooth for an aggressive restoration.
The biologic assessment is heavily weighted in determining the viability and acceptability of placing a single tooth implant. The next category essential to look at is structure, which is the condition of the adjacent teeth next to the potential pontic or implant site. Structural issues frequently suggest or diminish the option of choosing an FPD over an implant.
Structure — Are Adjacent Teeth Restored?
Are the adjacent teeth restored, or do they need restoration? Suppose the adjacent teeth are not restored and don’t need a restoration. In that case, it represents one of the significant advantages of a single tooth implant — the ability to replace the tooth without involving unrestored teeth.
If the adjacent teeth aren’t restored, and it is necessary to use an FPD due to the patient’s growth status, lack of bone, or inadequate space for an implant, a conservative bonded option is generally a better choice than one with full-coverage retainers. This is especially true if the lateral incisor is being restored, as it can often be cantilevered successfully from the canine4.
Even if the patient is in their 20s and requires single tooth replacement but won’t consider an implant, I prefer to use a bonded FPD if the adjacent teeth are unrestored. It won’t have the same lifespan as a conventional FPD, but it can always be replaced with a more definitive form of tooth replacement in the future; our methods of tooth replacement continue to improve with time.
If the adjacent teeth are restored and the restorations need to be redone, or if the teeth need restoration, the advantages of the implant are reduced. However, one could argue that having all single units is still enough reason to choose the implant (Figs. 11–13).



Structure — Condition of the Adjacent Teeth
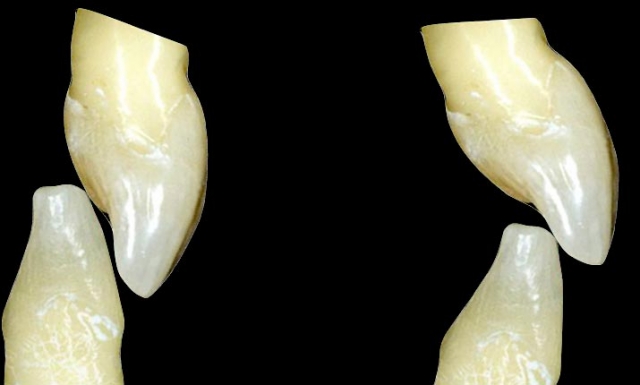
Is the condition of the adjacent teeth compromised to act as abutments for an FPD? Excellent clinical studies have compared the longevity of FPDs with and without non-vital abutments. These same studies have evaluated the longevity of single crowns on vital or nonvital teeth. There is very little difference in estimated 20-year survival rates for single crowns, 75% versus 79%. However, a non-vital abutment significantly decreases the estimated 20-year success of three-unit FPDs: 83% versus 60%5. The numbers even worsen for more than three-unit FPDs, or cantilever FPDs with a non-vital abutment (Figs. 14–16).


Structure — Which Tooth Is Being Replaced?
Suppose the lateral incisor is the tooth being replaced. In that case, the literature supports the claim that a cantilever FPD is a highly successful option, even when using a conservative bonded retainer. Dr. Kern reported a 94%, 10-year success rate with such restorations (Figs. 17–21). If, on the other hand, the centrals or canines are being replaced, a cantilever FPD is probably not a good option.




Functional considerations and concerns for single anterior tooth replacement are overbite/overjet relationships, mobility, and parafunctional habits.
Function — Overbite/Overjet (Deep Bite)
The concerns about the anterior relationship relate to the occlusal forces applied to the restoration and the room available for it.
There are deep bite relationships that are almost impossible to gain space for an implant, abutment, and final restoration. Additionally, if an implant is placed, it will make any future orthodontic correction of the occlusal relationship extremely difficult because the position of the implant would be related to the existing, less-than-ideal tooth position. Generally, I would avoid single tooth implants in intense bite situations, especially in younger patients.
Deep overbites also make bonding bridges extremely difficult because there is no room for the lingual wings without significant tooth preparation. Also, a deep overbite has been shown to reduce the lifespan of resin-bonded FPDs6 significantly.
The best alternative for patients with a missing anterior tooth and a deep overbite is orthodontics to correct the occlusal relationship, following orthodontics the single tooth implant or bonded bridge become more predictable (Fig. 22).
If the patient won’t consider orthodontics at this time, a full coverage FPD may be the most predictable option, but preferably out of a material that has adequate strength in thin sections to minimize lingual tooth reduction, such as metal, or Zirconia.
Function — Mobility
Tooth mobility levels can significantly affect the success of the different tooth replacement options. Mobility can result from excessive occlusal forces, inadequate root length, or unfavorable occlusal relationships. If the source of the mobility can be identified and controlled, then it is no longer an issue. If the mobility cannot be controlled, the clinician needs to know how it impacts the choice of tooth replacement.
Differential mobilities can be a recipe for a disastrous bonded FPD experience. If we choose to replace a missing lateral using a canine with a normal level of mobility as one abutment and the central abutment is excessively mobile, the least mobile tooth — in this case, the canine — will almost always be the one that de-bonds. In these cases, a cantilever off the canine is a much better choice than involving the central, whether it is a bonded or conventional retainer on the canine.
The outcome is much better when replacing a central using central and lateral abutments that are slightly mobile for a conventional three-unit FPD. When both abutments are equal in mobility, and when the direction they move under load is similar, as with a central and lateral, these restorations can be very successful long term. In fact, tying them to non-mobile canines only complicates the prosthesis and puts the canines at risk (Fig. 23).

Mobility’s impact on implants is a more complex story. If we replace a single central tooth with an implant, and the adjacent anterior teeth are mobile, they will move out of the way under load, and all the occlusion will now be on the implant. Suppose you use a single anterior implant in a patient with mobile anterior teeth. In that case, it is beneficial to be sure the teeth still provide most occlusal contacts during excursions to avoid the implant handling all the contact.
Function — Future Tooth Position Changes
As mentioned above, when discussing deep overbite, anytime you believe a change in anterior tooth position would benefit the patient from a functional perspective, you must be careful about using a single anterior implant because it will be positioned relative to the existing teeth. The placement of the implant will almost always compromise any future orthodontic corrections. In these patients, an FPD is often a better alternative.
Esthetics is the last area of concern, but it relates heavily to the already analyzed area of Biology. The esthetic outcome of a single tooth implant can be exceptional, but it depends entirely on the surrounding soft tissue, which depends on the underlying bone.
Esthetics — Patient Demands
Suppose the patient desires a structurally sound tooth replacement that leaves their adjacent teeth untouched, and is not critical esthetically. In that case, a single tooth implant is a great choice even if the final soft tissue result is an esthetic compromise.
If the patient has a high lip line, it is esthetically demanding and won’t accept compromise. The bone and soft tissue will need to be excellent for an acceptable single tooth implant (Figs. 24 and 25).


Esthetics — Predict a Realistic Esthetic Outcome and Present it Before Treatment
As much as implants have impacted dentistry over the last 30 years, they have their limitations. Even with many of today’s newest techniques for bone and soft tissue augmentation, we still can’t achieve ideal in many patients7.
When I discuss this with patients I often talk about what is surgically possible, as opposed to what is surgically predictable. As a general rule, when bone and soft tissue are compromised, it is much easier to produce an acceptable FPD from an esthetic perspective, even if it requires pink ceramic or composite, than a compromised single tooth implant.
The goal of this article isn’t to provide a cookbook as to whether a single tooth implant or FPD would be the correct choice, as that isn’t possible when dealing with patients and their highly individual behaviors and preferences. In fact, all treatment decisions are influenced by a variable I didn’t discuss: human emotion.
References
- De Rouck, T., Collys, K., & Cosyn, J. (2008). Single-tooth replacement in the anterior maxilla by means of immediate implantation and provisionalization: a review. International Journal of Oral & Maxillofacial Implants, 23(5).
- Salama, H., Salama, M. A., Garber, D., & Adar, P. (2001). The Interproximal Height of Bone: A Guidepost to Predictable Aesthetic Strategies and Soft-tissue Contours in Anterior Tooth Replacement. Craniofacial Growth Series, 38, 91-106.
- Snodell, S. F., Nanda, R. S., & Currier, G. F. (1993). A longitudinal cephalometric study of transverse and vertical craniofacial growth. American Journal of Orthodontics and Dentofacial Orthopedics, 104(5), 471-483.
- Kern, M. (2005). Clinical long-term survival of two-retainer and single-retainer all-ceramic resin-bonded fixed partial dentures. Quintessence International, 36(2).
- De, B. H., Van, M. G., Decock, V., & Van den, B. L. (2007). Long-term survival of complete crowns, fixed dental prostheses and cantilever fixed dental prostheses with posts and cores on root-treated teeth. Primary Dental Care, (4), 155-155.
- Williams, V. D., Thayer, K. E., Denehy, G. E., & Boyer, D. B. (1989). Cast metal, resin-bonded prostheses: a 10-year retrospective study. The Journal of Prosthetic Dentistry, 61(4), 436-441.
- Rocchietta, I., Fontana, F., & Simion, M. (2008). Clinical outcomes of vertical bone augmentation to enable dental implant placement: a systematic review. Journal of Clinical Periodontology, 35, 203-215.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Frank Spear
Date: October 29, 2018
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


