Clinical Remount Procedure: A Visual Guide
Despite all efforts to minimize error while fabricating removable prostheses, accumulated inaccuracy will inevitably add up. Often, this inaccuracy must be managed during the denture insertion with a clinical remount. While the absolute need to perform a clinical remount procedure for every patient has been debated, without a doubt, there are times when a removable case will need to be re-articulated. When a remount is necessary, remount casts will be required.
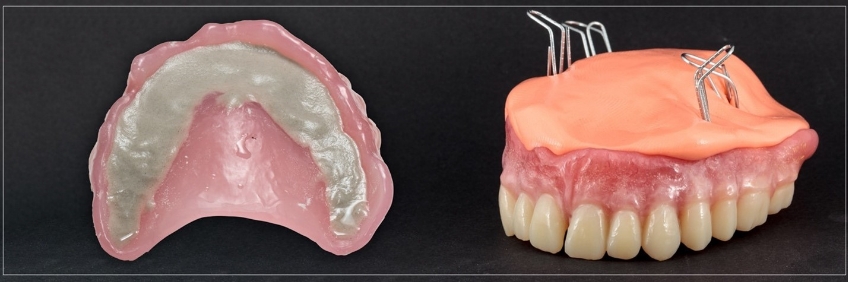
In the case of a new set of conventional dentures, the dental laboratory technician may have previously fabricated the remount casts, anticipating their potential need as part of the prescribed work (Fig. 1). However, there are several clinical scenarios in which the technician may not have provided the remount casts or the casts are unavailable.
In addition, while these casts are often referred to as “remount” casts, their utility far exceeds their name. For example, remount casts can be incredibly helpful during denture base repairs (Fig. 2) and when evaluating the patient for prosthetic space availability. In contrast, treatment planning for implants (Fig. 3). As a result, the fabrication of remount casts is a skill set many clinicians may want to know.



Clinical Remount Procedure: Techniques and Materials
The materials and techniques may vary slightly depending on the desired use of the cast. Regardless of intended use, in the first step, all undercuts on the prosthesis intaglio surface must be blocked out to preserve the ability to separate the denture and the cast without damage.
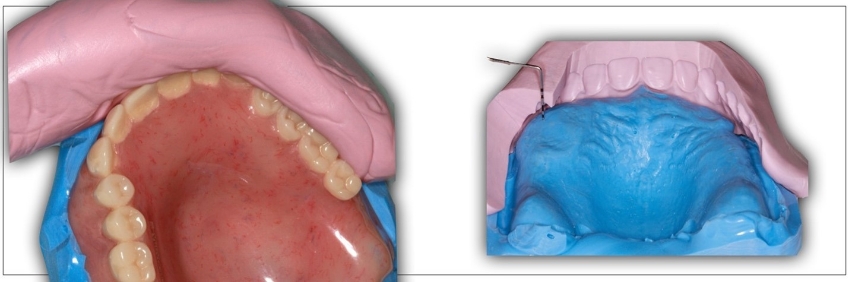
Classically, a medium grit pumice slurry (Pumice No.3, Kerr Corp.), modeling clay, or even a wet paper towel would be used for this step (Fig. 4). Another option is to use a silicone material, such as a lab putty Matrix Form 60, Anaxdent North America) (Fig. 4) or even a medium body polyvinyl siloxane impression material Examix Regular Type, GC America (Fig. 5).
The silicone fabrication option can preserve detail from the prosthesis intaglio that would otherwise be lost. Suppose silicone, either impression material or laboratory putty, is used. In that case, the material should be adapted well to the prosthesis’s intaglio surface and then allowed to set under 2-3 bar positive pressure (pressure pot, Great Lakes Dental Technologies).

Once the intaglio has been sufficiently managed, the next step is to create a rigid and stable base (Fig. 7). Generally, a Type II mounting stone (Mounting Stone, Whip Mix) is adequate for the base of the remount cast. A faster setting stone may be desired in specific clinical circumstances where time is critical, such as the need to repair a fractured denture base. Type I mounting plasters often set more quickly than Type II mounting stones, but lack the compression strength of Type II stones and experience significantly more setting expansion. As a result, Type I plaster is not an excellent option for improving efficiency. A better option would be selecting a rapid-setting, low-expansion Type IV stone (Snap-Stone, Whip Mix Corp.)

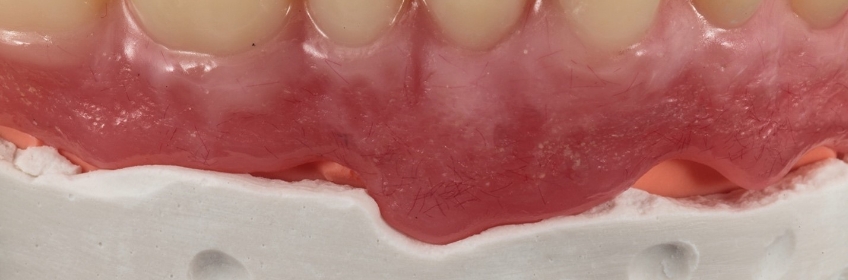
In a clinical remount procedure where the occlusion will be selectively adjusted, the denture must be stable on the remount cast. If silicone is used, it is essential to clear the silicone from the denture flange for the prosthesis flange to “bottom out” on the stone portion of the cast (Figs. 8 and 9). This is less of an issue if the cast will be used for space analysis.

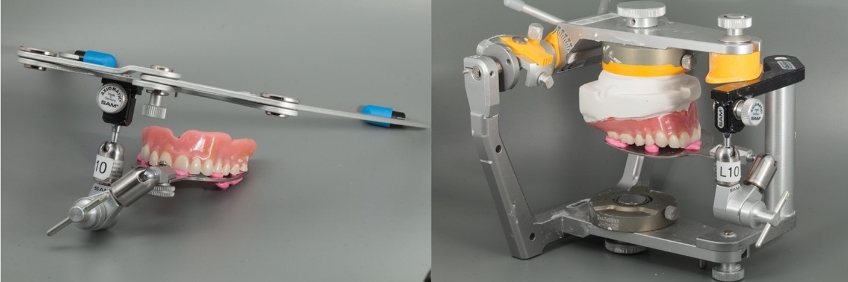
Once the stone has been set, the stone base is trimmed in the usual fashion and can be re-articulated in whichever manner the clinician chooses (Fig. 10).
The Value of the Clinical Remount Procedure in Practice
While the remount cast can undoubtedly help identify and manage occlusal inaccuracies with conventional complete dentures as part of a clinical remount procedure at the insertion appointment, the same type of cast may also be helpful in a variety of different applications that the clinician may face when working with edentulous patients. The techniques described in this article should provide clinicians with options for efficiently fabricating these casts in the office, thereby preserving clinical efficiency by not relying on their delegation to the dental technician.
References
- Firtell, D. N., Finzen, F. C., & Holmes, J. B. (1987). The effect of clinical remount procedures on the comfort and success of complete dentures. The Journal of Prosthetic Dentistry, 57(1), 53-57.
- Ansari, I. H. (1996). Simplified clinical remount for complete dentures. The Journal of Prosthetic Dentistry, 76(3), 321-324.
- Verhaeghe, T. V., Linke, B. A., Cable, C. E., & Mostafa, N. (2019). Clinical remounting of complete dentures: A systematic review. The Journal of Prosthetic Dentistry, 121(4), 604-610.
- Zarb, G. A., Hobkirk, J., Eckert, S., & Jacob, R. (2013). Prosthodontic treatment for edentulous patients: complete dentures and implant-supported prostheses. Elsevier Health Sciences.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Darin Dichter
Date: August 25, 2022
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


