Arg! Another Zirconia Crown Fell Off: A Guide to Recementing Crowns
Frustration echoed through the office as yet another zirconia crown fell off prematurely. This situation is a common occurrence for many dentists. Zirconia, valued for its strength and durability, can challenge achieving reliable adhesive retention. This article explores essential steps and protocols for effectively recementing crowns, offering practical solutions to prevent such issues in dental practices.
Common problems with recementing crowns
”Arg! Another zirconia crown fell off! I am so frustrated! It was recently cemented (December) with a universal self-adhesive cement. Why does this keep happening? And what can I do to prevent it from happening again?”
This aggravating and annoying situation comes from Ashley, one of our recent Restorative Design workshop participants. Unfortunately, this is a common and disturbing occurrence for many dentists!
Dr. Bob Winter and I hear this vexing scenario often. Zirconia crowns are one of the most used restorations by dentists. The following diagram provides insight into why many dentists choose zirconia as their restoration material.
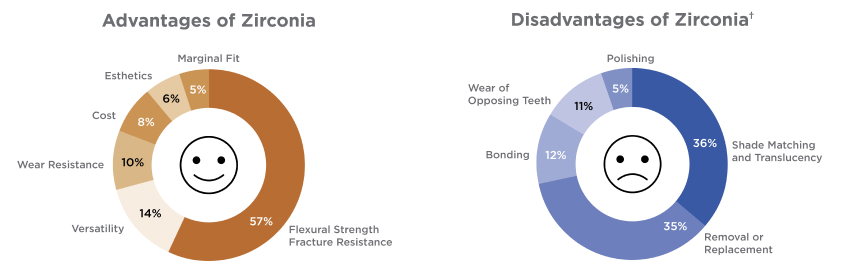
The latest ADA ACE Panel Report includes responses from 277 ACE Panel member dentists about how they use zirconia in their practices (ADA News, January 2021).
Zirconia is a strong and durable material for clinical use. However, adequate tooth reduction and surface preparation are required to attach to tooth structure predictably. As you can visualize from the diagram above, clinicians report that bonding to zirconia is considered a disadvantage. As such, most zirconia restorations are cemented. Regardless of the adhesion method chosen, definitive protocols and processes must be detailed and applied to achieve the most predictable and long-lasting results when recementing crowns.
Zirconia restoration insertion:
Key protocols for success
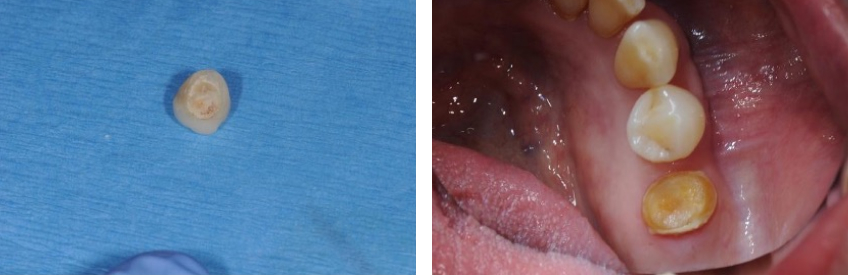
When a previously cemented restoration comes off prematurely, it’s crucial to observe where the old cement remains attached. This observation can provide clues to the origin of the breakdown. If cement is found within the restoration’s intaglio, it suggests that the tooth surface may not have been adequately prepared before cementation. Conversely, if the cement remains on the tooth, it indicates potential issues with the restoration preparation.
Regardless of the situation, the restoration and the tooth must be thoroughly cleansed and managed to establish a durable connection. The following steps outline how to ensure accuracy when recementing crowns:
Try-in and check margins
The marginal fit and contacts of the restorations are evaluated on the prepared tooth. Any contact adjustments are done, and the surface is actually polished. Occlusal adjustment should be minimal until the restoration adheres to the tooth. Adjustments are ideally performed with a fine diamond at low speed (less than 20,000 RPM) and then polished to a high shine. Using a handpiece at high speed creates flaws in the ceramic, which can lead to early fracture. Even if the zirconia is 3Y (and, to a lesser degree, 4Y) and can undergo transformational toughening, thereby limiting crack propagation, multiple high-speed applications create a limit to minimizing internal flaws. Crack defects and fractures can occur because of continued ceramic adjustments.
Air-abrade tooth with 25- to 50-micron alumina oxide
The tooth structure must be cleansed and free of biofilm and provisional cement debris before the adhesive process. These products will interfere with the adhesion of restorations to the tooth structure and result in potential early and undesirable dislodgment. The best way to debride the tooth surface is micro air abrasion with 25- to 50-micron alumina oxide particles. The second-best alternative is a slurry of pumice and a rubber cup.
Properly isolate tooth
Once the tooth is cleansed, it must be isolated appropriately to avoid contamination with saliva and crevicular fluids. Rubber dams, “Isolite,” etc., are good retraction and evacuation devices. Cotton rolls can also be effective. Retraction cords and hemostatic agents are often necessary to remove gingival tissue interference and control any hemorrhage that may have occurred during tooth cleansing/air abrasion.
Clean intaglio of restorations
The inner surface of the restoration must be thoroughly cleansed. Organic contaminants will interfere with the zirconia’s ability to interact with the adhesive. Zirconia has a high affinity for blood, lipids, saliva, and proteins from the try-in phase. The best method for cleansing the restoration is micro air abrasion with 25- to 50-micron alumina oxide particles. This process provides a clean surface and incorporates a micromechanical roughness for cement interaction.
It is best to air-abrade the surface just before the adhesive process, because the surface is then “positively charged” and provides surface energy that ensures more intimate priming capability. The restoration does not need to be rinsed after air abrasion; air flow will remove the excess alumina particles.
Alternatively, there are a variety of chemical agents specifically designed to clean and prepare the intaglio aspects of ceramic restorations. Products like Ivoclean (Ivoclar), Katana Cleaner (Kuraray), and ZirClean (Bisco) all remove the organic contaminants of blood and saliva. Follow the manufacturers’ directions to ensure proper surface preparation.
Prime the zirconia surface
The surface of the zirconia must be activated or primed to create a chemical adhesion for the resin cement. Ceramic primers are designed for this purpose. The magic ingredient enabling this chemical connection to zirconia is 10-MDP monomer. Zirconia lacks glass particles, so etching the surface with hydrofluoric acid (common for glass ceramics like lithium disilicate) is unnecessary and ineffective. Monobond Plus (Ivoclar), a universal primer containing both 10-MDP and silane, is widely used for priming both zirconia and glass ceramics. If the crown was cleansed with a specific chemical cleanser containing 10-MDP, such as Katana Cleaner or ZirClean, the surfaces are primed and ready for adhesive.
Multiple applications are recommended when applying primers, agitating each for 2 minutes. Solvent should be allowed to evaporate, followed by air-thinning to ensure complete solvent dissipation. It’s important to note that Monobond Etch and Prime (Ivoclar) is not intended as an adhesive activator for zirconia, because it contains silane rather than 10-MDP, and is designed for priming glass ceramics.
Adhesive resin application
An adhesive resin is now applied to the primed intaglio surface. The purpose of the resin is to provide a ”wetted” surface to facilitate better cement distribution. If the adhesive resin is a universal adhesive, it likely contains 10-MDP. Priming the zirconia restoration should still be conducted as a separate step. Universal adhesives contain various chemical ingredients and a significant amount of water to initiate chemical reactions for adhesion to enamel and dentin. It is well documented that additional primers, such as 10-MDP and silane, may be deactivated by the complex chemistries and interactions occurring with universal resins. Scotchbond Universal (3M) exemplifies one of many adhesive resins. The resin is applied in a thin layer to the intaglio of the crown. I do not light-cure this applied layer.
A thin adhesive resin layer should also be applied to the prepared tooth structure. This step allows for dentin sealing. The literature recommends air-thinning this adhesive layer and complete light activation (cure). Polling dentists at the ARD Workshop, it is common practice not to cure this resin layer before the cementation process. The consensus and reason for this approach are concerns about improper or incomplete seating of the restoration due to resin thickness. A more viscous adhesive resin may exacerbate these concerns. Due to free radical activity, the uncured adhesive resin will harden under the restoration upon light activation. Again, Scotchbond Universal (3M) is among the many resin adhesives that may be used. If left uncured, it will also aid in the distribution of cement upon restoration insertion.
Cementation
Cementing (versus bonding) is the most widely used process of adhesion for zirconia restorations. Adequate resistance and retention form of the tooth preparation allow for predictable cementation and restoration longevity.
Most clinicians prefer to cement zirconia rather than adhesively bond it. But if the protocols outlined above are followed precisely, the adhesive connection to zirconia is predictable.
Most dentists use RMGI or a self-adhesive cement as the luting agent for zirconia. Both are acceptable choices. If RMGI is used, the cement is allowed to cure (approximately 2 minutes; always follow manufacturers’ instructions). The excess is then removed.
Alternatively, if a self-adhesive luting agent is used, the material is dual-cured. For instance, if Rely-X Universal Self-Adhesive (one of many alternative products) is used, the cement is applied to the restoration’s intaglio and distributed evenly in a thin layer. The restoration is seated on the tooth preparation.
Before removing the excess, a spot-cure approach is used to initially harden the excess around the restorative margins (3–5 seconds). The excess is then nudged with the end of an explorer to break away or separate it from the marginal area. The entire excess is not removed at this time!
Once nudged, the cement is fully cured by light activation and allowed to self-cure (follow manufacturers’ instructions). The hardened excess cement is then removed completely.
Occlusal adjustment
The now-luted restoration can be adjusted for any occlusal interferences that may be present. A fine diamond with low speed (20,000 RPM) is the recommended instrument and method of adjustment. This speed and grit will allow for minimal scratching and minimize the initiation of microflaws within the ceramic. Microcracks are possible depending on the type of zirconia. For instance, in 3Y zirconia, crack propagation is limited due to transformational toughening (“crack limiting”).
Alternatively, with 4Y zirconia, the literature supports that initial occlusal adjustment may initiate the zirconia “crack limiting” process (depending on the alumina percentage within the zirconia itself), but continued or extensive adjustment can cause internal ceramic flaws and cracks. Care must be taken to avoid extensive adjusting procedures on any ceramic. Ceramic polishing measures must follow any ceramic occlusal adjustment. Well-polished zirconia is the most favorable ceramic surface for opposing natural tooth surfaces.
I hope this explanation of the zirconia cementation sequence is helpful to those of you who may be having problems or concerns about recementing crowns.
References
- Lawson, NC, Maharishi, A. (2020). Strength and translucency of zirconia after high‐speed sintering. Journal of Esthetic and Restorative Dentistry, 32(2), 219-225.
- Mehari, K, Parke, AS, Gallardo, FF. (2020). Assessing the effects of air abrasion with aluminum oxide or glass beads to zirconia on the bond strength of cement. The Journal of Contemporary Dental Practice, 21(7), 713-717.
- Sulaiman, TA, Suliman, AA, Abdulmajeed, AA, Zhang, Y. (2024). Zirconia restoration types, properties, tooth preparation design, and bonding. A narrative review. Journal of Esthetic and Restorative Dentistry, 36(1), 78-84.
- McLaren, EA, Maharishi, A, White, SN. (2023). Influence of yttria content and surface treatment on the strength of translucent zirconia materials. The Journal of Prosthetic Dentistry, 129(4), 638-643.
FOUNDATIONS MEMBERSHIP
New Dentist?
This Program Is Just for You!
Spear’s Foundations membership is specifically for dentists in their first 0–5 years of practice. For less than you charge for one crown, get a full year of training that applies to your daily work, including guidance from trusted faculty and support from a community of peers — all for only $599 a year.

By: Jeffrey Bonk
Date: July 30, 2024
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


