Post-Pandemic Dentistry: Bruxism, Tooth Wear, and Communication

Editor’s Note: In September 2020, the American Dental Association Health Policy Institute released findings from an impact poll highlighting an increase in certain oral health conditions since the onset of the COVID-19 pandemic. Doctors who participated in the ADA poll reported increases in bruxism (54.9%), chipped and cracked teeth (53.4%), temporomandibular disorder symptoms (53.4%) and caries (26.4%) among patients. In this series, Spear faculty explore what clinicians and practice teams must know to successfully treat these four conditions on the rise.
The etiology of bruxism — both clenching and grinding — has been debated for decades. For much of the past 50 years, many dentists were taught that bruxism occurred because of a patient’s occlusion not being correct, and that if the occlusion was corrected, the bruxism would stop.
The vast amount of research published over the past century does not substantiate those beliefs.1 Instead, it appears that bruxism can occur due to multiple different etiologies, including sleep apnea,2,3 airway issues not involving an apneic event,4 medication-induced bruxism,5 and stress-related incidents.6,7
In fact, there is research done where students’ salivary cortisol levels were measured before being given a stressful math equation to solve, then measured immediately after the stress test, and measured again 10 minutes later.
If the subjects were asked to clench on their anterior teeth on and off for the 10 minutes after being stressed, they could lower their salivary cortisol levels very rapidly,8 indicating that clenching and grinding may be a method of stress relief — which is most likely what is happening from the pandemic.
It’s also interesting to note that the incidence of nocturnal bruxism decreases with age, peaking at 20% in children 11 and younger, dropping to 13% for young adults between 18 and 29, and reducing to 3% in adults over 60. In contrast, daytime bruxism increases from 12% in children to 20% in adults.9 The force applied during daytime clenching and grinding can also be significantly greater than that applied at night.10
The importance of early bruxism diagnosis and treatment
Bruxism, either clenching or grinding, can result in many different outcomes for our patients. These range from increased incidence of TMD symptoms to chipping and fracturing of teeth, and from tooth grinding, the potential for significant tooth wear.
The challenge for clinicians is that in many patients who brux, they have no obvious symptoms unless there has been a tooth fracture or they’re experiencing TMD. Said differently, unless the wear is severe, many patients will be unaware it is occurring. This means the clinician must develop the skills of learning to present the long-term negative consequences that may occur from bruxism to the patient.
Using the co-diagnostic case presentation method for patients with tooth wear
In both our Treatment Planning With Confidence workshop and the Art of Treatment Planning and Case Acceptance seminar, we teach the co-diagnostic approach to case presentation developed by the late Bob Barkley. It is an essential tool to learn when discussing things such as tooth wear in patients who are unaware. The steps in co-diagnosis are quite simple. Let’s look at each of them in-depth here.
Showing patients what you see
Step 1 involves making the patient aware of the problems you see. For patients with tooth wear or teeth chipping, this is usually done with photography. Until a patient realizes they have a problem, they will have no reason to treat it. However, simply becoming aware that the problem exists typically does not motivate the patient to go forward and ask for treatment.
Illustrating the consequences of inaction
Step 2 in the co-diagnostic process is critical because it makes the patient aware of the potential consequences of not moving forward with treatment. For patients with bruxism who are experiencing TMD symptoms, getting them to want treatment is easy because they want to feel better. For patients with asymptomatic tooth wear, getting the patient to want treatment will depend upon the clinician painting a vivid picture of what happens when tooth wear is left untreated.
If you’re a Spear member and have access to our dental patient education platform, the short lobby video Understanding Tooth Wear illustrates the potential consequences of untreated tooth wear in less than two minutes. If you don’t have access to the patient education videos, using photos of other patients with severe untreated wear can be very effective at educating patients about future consequences.
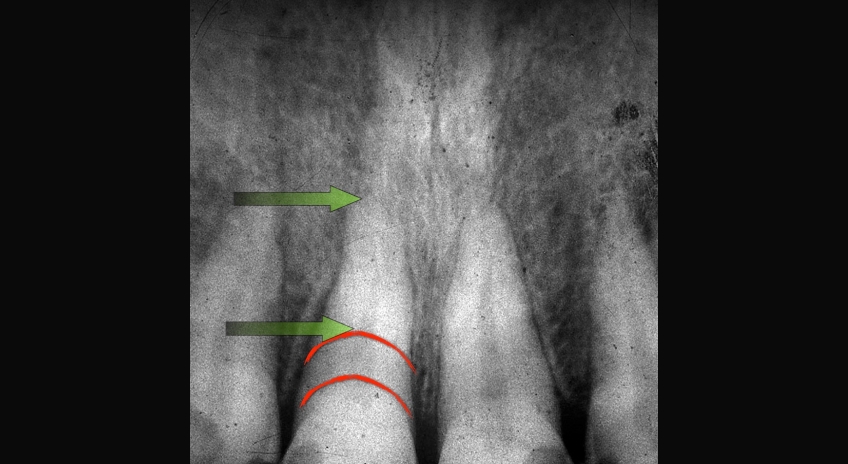
Your discussion should highlight the fact that as wear progresses, it will spread to more and more teeth in the mouth, making the potential treatment far more complex and expensive. It is also important to acknowledge that as tooth wear progresses, the teeth will often move — erupt, if you will — from dentoalveolar extrusion to maintain occlusal contact. This means the teeth are getting shorter and shorter and future treatment may involve possible crown lengthening to reposition gingiva and bone to expose more tooth (Figs. 1–5). If crown lengthening is necessary for a patient, Spear members can use the patient education video Crown Lengthening (Tooth Wear), which illustrates this well.
Often the alternative to crown lengthening is orthodontic intrusion to move the teeth, gingiva, and bone back to their correct position, allowing for restorations to be placed. This is covered in the patient education video Orthodontic Intrusion available to Spear members.





Ideally, in Step 2 of co-diagnosis the patient has an emotional response when they realize what having the problem means for the future if no treatment is done. The ideal outcome when you’re done with Step 2 — and have explained the consequences of doing nothing — is to have the patient ask, “What can be done?”
Explaining the benefits of treatment
Step 3 in co-diagnosis is explaining the benefits of treatment. This step is not about presenting a treatment plan; it’s about explaining how the patient’s prognosis will change if they move forward with treatment.
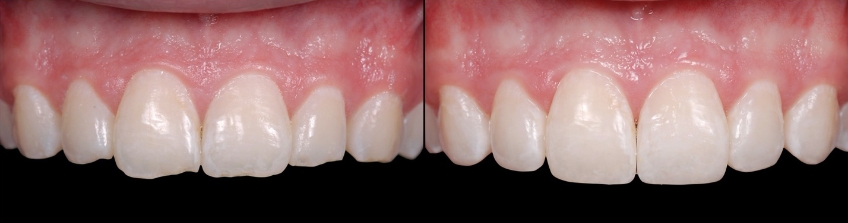
For most wear patients, moving forward with treatment means placing some type of restorations on the worn teeth — the benefit of placing the restorations is that their natural teeth are now protected from any future wear by the restorative material. Additional benefits are typically enhanced esthetics as well.
It’s important to note that our treatments can be very successful at protecting the teeth, but that doesn’t mean the patient will stop their bruxing behavior. It is possible that the restorations may need some maintenance in the future, but the patients will have their own healthy teeth underneath.
Presenting treatment options
The final step in co-diagnosis is presenting treatment options to the patient. Again, this is not presenting a treatment plan that you developed; this is helping the patient co-select and develop the plan with you.
Examples of treatment options may be crown lengthening vs. intrusion to reposition overerupted anterior teeth (Figs. 6–10). You can explain each — or show the Spear Patient Education videos of each — then discuss with the patient why you believe one may be better for them.
Other options may be the use of direct composite vs. an indirect type of restorative approach. For many patients, direct composites have significant advantages because they require minimal if any tooth preparation, hold up extremely well, are easy to repair, and cost significantly less than the same number of indirect restorations.
Direct composite onlays can also be used very predictably on posterior teeth in patients who need their vertical dimension increased. Our Worn Dentition workshop takes you through which patients need their vertical changed, which teaches you how to identify the amount of change required. You also learn to fabricate direct composite onlays to increase the vertical and how to place them.




What to do now in your practice
Perhaps the most important thing to do now is to realize the increase in bruxism, chipped and fractured teeth, and TMD is occurring from the pandemic. You may consider implementing a simple addition to your dental health and jaw joint history with questions that help a patient identify if they find themselves clenching and grinding more often or having symptoms of TMD.
If you see a patient who’s started to notice an increase in bruxism or chipping and fracturing teeth, you want to discuss it — and be supportive that they are not unique. There’s a large increase in such behaviors from the pandemic.
What about treatment?
Clinicians tend to want to prescribe a nightguard for patients who clench and brux, which is logical, but limited in its effectiveness because more adults are clenching and grinding during the day than they are at night, and they aren’t wearing the nightguard during the day.
Would I still prescribe a nightguard? Yes. What type of nightguard is a more difficult question to answer without having all the details on a patient, and we must recognize different patients respond differently to the same type of appliance.
As a rule, a full-coverage, relatively flat-plane appliance is safe for almost everybody. Realize that there are studies that show 20% of patients with sleep bruxism have increased EMG activity during sleep while wearing an appliance, especially the soft mouthguard-type appliances.11 You can learn more about this in our Occlusion in Everyday Practice seminar.
For most patients with tooth wear, the ideal treatment involves restorations to protect the worn teeth and learning how to idealize the patient’s occlusion. As I wrote earlier, we used to believe that idealizing the occlusion would stop the bruxing behavior, which we now know is rarely true. However, learning how to develop an occlusion that distributes the load from the bruxism correctly and simultaneously over multiple teeth, can create an outcome that predictably survives even in patients who continue to brux.
As mentioned earlier, worn teeth typically don’t have indirect restorations, but amalgams or composites instead. This makes them easy to bond to, so you can create and try out your treatment plan with minimal to no tooth preparation and at a reasonable cost for the patient (Figs. 11–14).



The other area that’s important to address when discussing bruxism is the airway component, because in many patients, airway is the primary etiology. What this means for your practice is getting educated in screening and diagnosing bruxing patients to identify those who may be at risk due to the role of airway in their condition.
This can involve learning when a full-blown sleep study should be done. We have multiple online courses on the topic, and Dr. Jeff Rouse teaches our hands-on workshop, Airway Prosthodontics and Sleep Dentistry: Prevention to Control, as well as our Airway Prosthodontics: Just Do Dentistry seminar.
Final thoughts
The anxiety created from the pandemic has certainly affect all our lives, some with much more stress than others, and it’s not surprising our profession is seeing more stress-related behaviors such as bruxism, chipping and fractured teeth, and TMD. It’s unlikely this stress level is going to subside quickly, and learning how to diagnose, treatment plan, and treat these patients in need can be incredibly rewarding for them — as well as you and your practice. I encourage you to hone your skills and knowledge so you start to become comfortable with these patients’ needs.
And please, if you do see patients come in who are obviously starting to decline and experience wear, chipping, or fractures, use the co-diagnostic model to talk to them — don’t just present a treatment plan that scares them away.
I much prefer having these conversations as soon as you recognize what’s happening, and I also prefer early intervention with direct composite to virtually any other treatment method. The last thing I’d want you to do is to tell your patient you’re going to “watch” or “monitor” their problem. If they’re bruxing, the problems will always get worse.
References
- J Prosthet Dent. 1999 Dec;82(6):704-13. Sixty-eight years of experimental occlusal interference studies: what have we learned? Clark GT, Tsukiyama Y, Baba K, Watanabe T.
- Int J Pediatr Otorhinolaryngol. 2004 Apr;68(4):441-5. Improvement of bruxism after T & A surgery. DiFrancesco RC, Junqueira PA, Trezza PM, de Faria ME, Frizzarini R, Zerati FE. Source: Division of Otolaryngology, São Paulo University Medical School, Rua Guarará 529 cj. 121, São Paulo CEP 01425-001, Brazil.
- J Oral Rehabil. 2008 Jul;35(7):476-94. Bruxism physiology and pathology: an overview for clinicians. Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Faculty of Dentistry, Surgery Department, Pain, Sleep and Trauma Unit, Université de Montréal, Hôpital du Sacré-Coeur de Montréal, Montréal, Canada.
- J Oral Rehabil. 2015 Nov;42(11):810-8. Epub 2015 Jul 1. Could transient hypoxia be associated with rhythmic masticatory muscle activity in sleep bruxism in the absence of sleep-disordered breathing? A preliminary report. Dumais IE1, Lavigne GJ1,2, Carra MC1, Rompré PH1, Huynh NT1.
- J Clin Psychiatry. 1993 Nov;54(11):432-4. SSRI-associated nocturnal bruxism in four patients. Ellison JM, Stanziani P. Department of Psychiatry, Tufts/New England Medical Center, Boston, Mass. 02111.
- J Prosthodont Res. 2011 Jul;55(3):159-64. Epub 2011 Feb 5. Clenching occurring during the day is influenced by psychological factors. Endo H, Kanemura K, Tanabe N, Takebe J. Source: Division of Fixed Prosthodontics, School of Dentistry, Iwate Medical University, 1-3-27 Chuodori, Morioka, Iwate 020-8505, Japan.
- Aust Dent J. 2004 Jun;49(2):84-9. Psychic and occlusal factors in bruxers. Manfredini D, Landi N, Romagnoli M, Bosco M. Department of Neuroscience, University of Pisa, Italy.
- J Prosthodont. 2007 Mar-Apr;16(2):129-35. Influence of chewing and clenching on salivary cortisol levels as an indicator of stress. Tahara Y1, Sakurai K, Ando T.
- Lavigne GJ, Manzini C. Bruxism. In:Kryger M, Roth T, Dement W (eds) Principles and Practice of Sleep Medicine. 4th ed. Philadelphia, Pa: W.B. Saunders Company; 2005: 946-959
- J Oral Rehabil. 2001 May;28(5):485-91. Quantitative study of bite force during sleep associated bruxism. Nishigawa K, Bando E, Nakano M. Department of Fixed Prosthodontics, The University of Tokushima, School of Dentistry, Tokushima, Japan.
- Dent Clin North Am. 2012 Apr;56(2):387-413. Sleep bruxism: a comprehensive overview for the dental clinician interested in sleep medicine. Carra MC, Huynh N, Lavigne G.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Frank Spear
Date: October 15, 2021
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


