Options for Determining Vertical Dimension With Edentulous Patients, Part 2
In a previous article, we discussed some of the most common techniques for determining the occlusal vertical dimension (OVD) with an edentulous patient. That article addressed some advantages and disadvantages of relying on pre-extraction records and suggested that clinicians should feel confident in evaluating and/or determining OVD using post-extraction techniques.
The most common post-extraction technique for determining OVD is the freeway space approach. However, this technique is not without its own set of challenges, and, as a result, it is helpful for the clinician to be familiar with additional post-extraction approaches. This article will describe several additional approaches to determining the OVD to build the clinician’s confidence in managing edentulous patients.
Following the Existing Dentures
When the patient presents with dentures, a common approach is to utilize the OVD of the existing dentures along with the freeway space approach.
With the dentures inserted, have the patient relax (physiologic rest position) and evaluate the interocclusal distance present between the maxillary and mandibular premolars. If the space is less than 2.0 mm, the OVD may be excessive for these dentures. If the interocclusal space is greater than 4.0 mm, the OVD may be deficient. If, in fact, the measured interocclusal space falls between 2.0 and 4.0 mm, it is correct.

The primary risk to this approach is assuming the OVD of the existing dentures is correct and simply following it in a perfect world, which may have been true when the dentures were initially fabricated. But in clinical reality, the denture teeth wear and the supporting tissues resorb, altering the current OVD from the OVD established at the time of insertion. What you and I would typically see then is an OVD that is deficient in an existing set of dentures.
Additionally, most patients demonstrate slight variability in the position of physiologic rest and the rest position may be significantly influenced by the presence or absence of the dentures during the evaluation. As a result, the existing dentures can give the clinician insight into the desired OVD, but the existing dentures should not be followed blindly. Rather, a combination of following the existing dentures and utilizing the freeway space approach provides a more predictable method for determining the desired OVD.
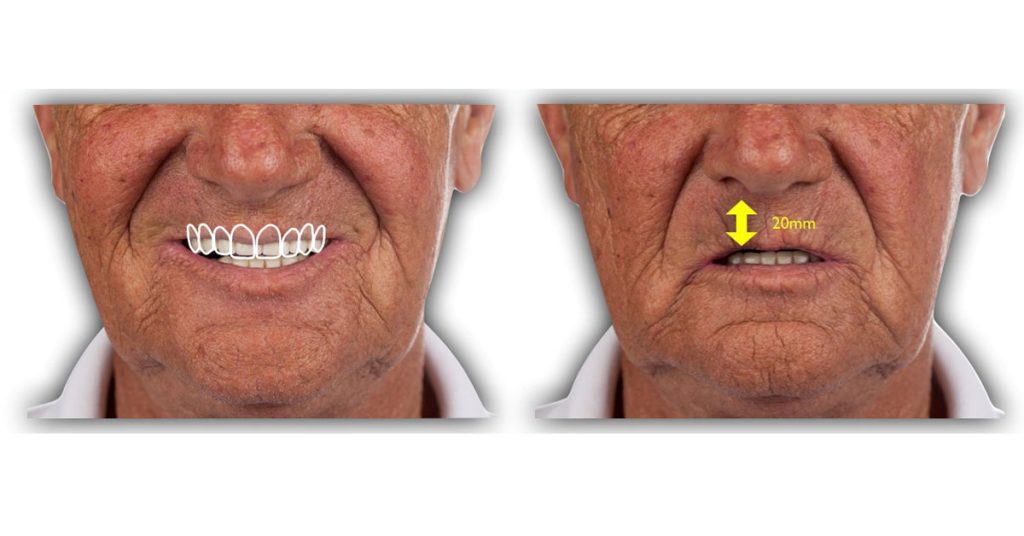
Facial Esthetics
Classically, the esthetic approach to establishing or evaluating the OVD begins with evaluating the vertical proportion of the face. Specifically, the lower 1/3 of the face relative to the middle 1/3 of the face. An ideal OVD would achieve a normal facial proportion of near 50% to 50% or slightly greater lower 1/3 relative to middle 1/3. A common finding with existing denture wearers is the lower 1/3 of the face is actually deficient relative to the middle 1/3, indicating a deficient OVD.
Phonetics
The phonetic approach to OVD determination is an extension of the concept discussed previously for determining the position of physiologic rest using the /M/ sound and then subtracting 2.0 to 4.0 mm to find the OVD. This approach uses the /O/ and /E/ sounds similarly. In a 2015 paper, Marko and colleagues describe asking their patients to pronounce the letter /O/ and subtracting 5.5 mm, and the letter /E/ and subtracting 7.5 mm to establish the desired OVD.
This approach has two challenges. The first is variability in the way individuals pronounce vowels across different languages and, as a result, this technique may require further evaluation to assess universal validity. The second challenge is how the clinician would measure the distances while the patient is pronouncing the vowels. Despite these challenges, this is an efficient approach to validate or test an initial OVD established with another technique.
Swallowing
Determining the OVD with the swallowing approach relies on the idea that as the patient swallows, the mandible moves from the physiologic rest position to where the teeth contact. If you try this on yourself right now, you will typically find that your teeth come into contact as you swallow, so that it would make sense.
The classic approach required using soft wax on record bases and asking the patient to swallow. Due to the difficulty of managing the wax and the variability in duration and intensity of swallowing, multiple authors have concluded that this approach may be best used clinically to verify OVD rather than the initial determination.

Craniofacial Landmarks
An extension of the esthetic approach, the craniofacial landmark approach uses information from the face to approximate the desired height of the lower 1/3 of the face, and as a result, the desired OVD. Several landmarks, as well as measurements between anatomic landmarks, have been proposed.
As an example, the maxillary incisal edge position would be determined based on the desired tooth display at rest and the length of the upper lip. The lower incisal edge position would then be determined based on the desired tooth display relative to the lower lip. And finally, the OVD would be established based on the desired vertical overlap of the anterior teeth (exactly how we teach clinicians to establish the OVD for dentate patients in our Vertical Dimension and Wear Spear Online course).
One of the big advantages of this approach is its esthetic predictability. The challenge with this approach is that most clinicians don’t set their own denture teeth and find it difficult to translate this desired OVD to the laboratory technician. As a result, it is a great approach for natural teeth but somewhat more difficult than some of the other approaches described when working with edentulous patients.
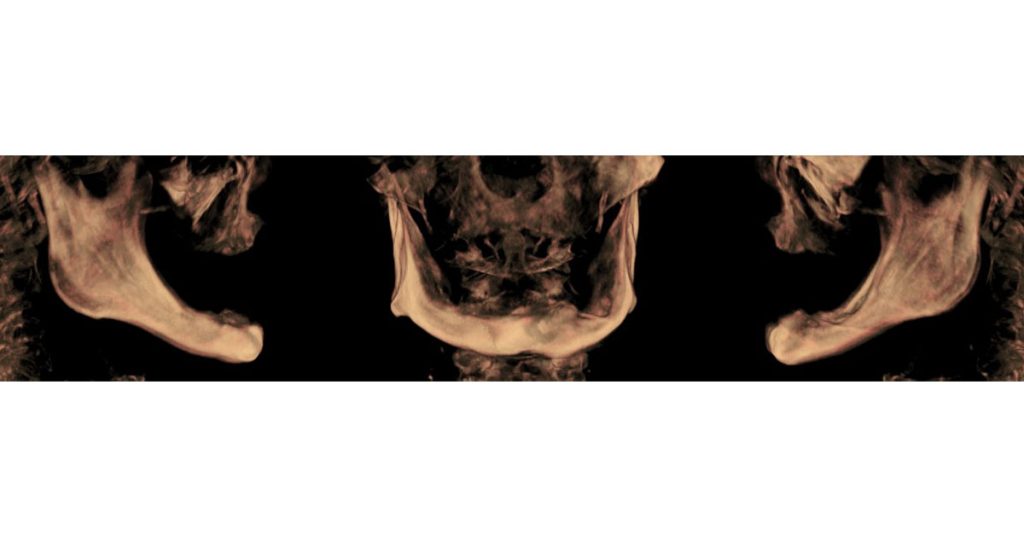
Cephalometric Evaluation
Using cephalometric landmarks to determine OVD is based on the idea that specific cephalometric landmarks do not change following edentulation. While certainly advantageous from an evaluation standpoint, the cephalometric approach has suffered historically from its lack of practicality.
That may be changing in the future as low-exposure CBCT protocols and virtual articulation have become routine in restorative practice, radiographic landmarks may become increasingly valuable in predictable determination of OVD.
Additional Methods
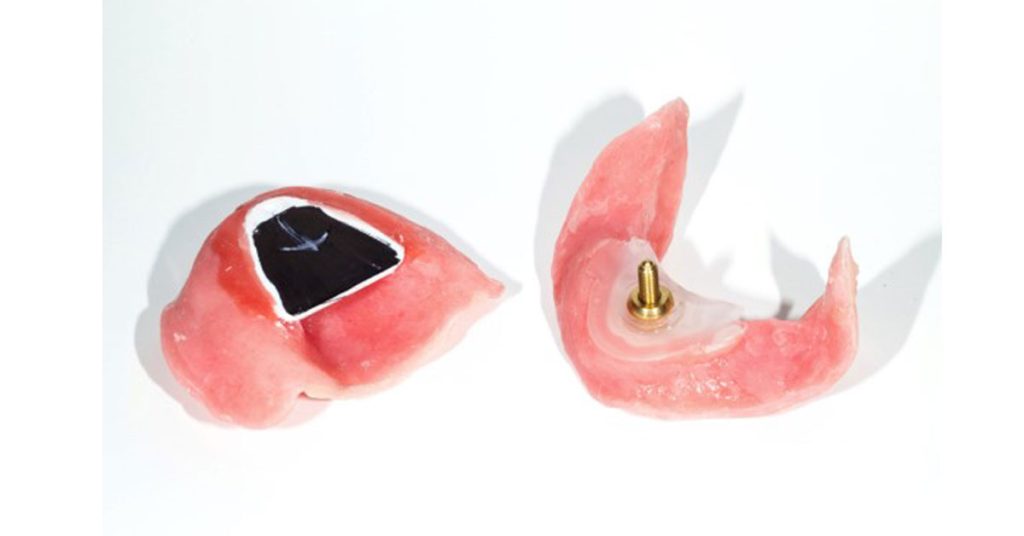
There is a long list of additional methods for determining OVD. While the previous methods are the most common, clinicians should know that other options exist. From determining OVD based on finger length to the capacity to generate bite force, these methods cover the spectrum from pragmatic to preposterous. One approach, however, does merit discussion: the tactile approach.
The tactile approach uses information from the patient directly to guide the clinician. Utilizing a device with an adjustable jackscrew, like an intraoral tracer, the OVD is gradually altered based on feedback from the patient. Experienced and even new denture wearers often feel that the bite is too “tall” or too “short.” Based on what the patient is experiencing, the length of the jackscrew may be increased or decreased.
The big advantage with this approach is that it engages the patient in their treatment and allows them to partner with their clinician in the evaluation and determination of the desired OVD.
The Best Approach?
Which method is the “best?” In truth, any one of the methods described in these articles could work for an individual patient, but none of the approaches presented will work with every patient, every time. As a result, in order to feel maximum confidence moving forward with an edentulous case, it is extremely helpful to be familiar with multiple approaches to determining the occlusal vertical dimension.
For many patients, it may be appropriate to establish an initial OVD based on the “freeway space” and “following the existing dentures” methods and then confirm the desired OVD with the “facial esthetic,” “phonetic,” and “swallowing” approaches. Finally, engage the patient using the “tactile” approach. If the OVD doesn’t feel good to the patient, clinicians are better off altering it in the wax rim or trial denture stage rather than after the prosthesis goes to final fabrication.
References
- Alhajj, M. N., Khalifa, N., Abduo, J., Amran, A. G., & Ismail, I. A. (2017). Determination of occlusal vertical dimension for complete dentures patients: an updated review. Journal of Oral Rehabilitation, 44(11), 896-907.
- Academy of Prosthodontics. (1999). The Glossary of Prosthodontic Terms. Mosby.
- Turrell, A. J. W. (1972). Clinical assessment of vertical dimension. The Journal of Prosthetic Dentistry, 28(3), 238-246.
- Igić, M., Krunić, N., Aleksov, L., Kostić, M., Igić, A., Petrović, M. B., … & Igić, A. (2015). Determination of vertical dimension of occlusion by using the phonetic vowel” O” and” E”. Vojnosanitetski pregled, 72(2), 123-131.
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Darin Dichter
Date: July 18, 2019
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


