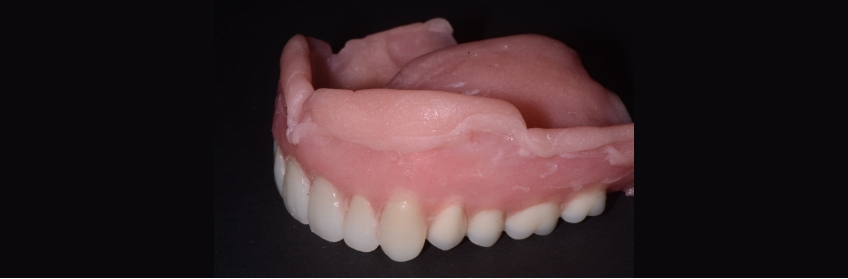
A Primer on Soft Denture Liners
Soft denture liners are as ubiquitous in removable prosthetic dentistry as dentures. We have been using these materials for more than a century and accept that none of the liners have a life expectancy comparable to that of a resin denture base.
Their purpose is to temporarily relieve sore tissues, help condition and provide retention, and distribute load more evenly on denture-bearing areas. For patients with thin atrophied ridges, bony undercuts, and non-resilient mucosa, a soft-tissue liner may be the only way a denture can be worn comfortably. We routinely place a soft liner on an immediate prosthesis, over a recent implant surgical site, or to help relieve tissue in cases of xerostomia. Clinical experience indicates almost universal tissue tolerance and patient acceptance.

The Categories of Soft Denture Liners
These resilient lining materials fall into one of two categories:
- The plasticized acrylic resins contain an acrylic monomer and plasticizers (ethyl alcohol and/or ethyl acetate), which preserve the material’s softness. The plasticizers are not bound within the resin and, therefore, will leach out in time.
- The silicone elastomers are polydimethylsiloxane polymers, similar to the silicone impression materials you may use. This helps retain the liner’s elastic properties for longer periods of time. However, they lack the leachable plasticizers (and aren’t as soft) that the acrylic resins have.
These soft denture liner materials have disadvantages: They are porous and not color stable, have low resistance to abrasion and short-term resiliency, and lack bond strength despite the chemicals applied to address this. The most common reason for the failure of a soft-lined denture is adhesion to the acrylic base.
Given enough time, wearing a denture will cause changes in the denture-bearing tissues. Utilizing a soft liner will improve the comfort and concomitantly the masticatory efficiency for most patients. For patients with insufficient ridge height or dry, thin tissues, the routine placement (and replacement) of liners may be the only way a denture can be worn. These liners will often act as masticatory shock absorbers.
The Right Liner for the Right Patient
I utilize both of these types of soft liners depending on what issue the patient presents with.
The plasticized acrylic resins (think Coe Soft, Coe Comfort) have polyethyl methacrylate powder, esters, and alcohol, but no methacrylate monomers. This material is soft but short-term (three to six months). I use it on immediate denture patients to surgically help with the retention and comfort post. The plasticizers will keep the liner soft for several weeks, but over time, the material hardens and must be replaced. I will add material every seven to 10 days until the immediate denture patient is comfortable and feels the denture is retentive enough. This can usually be achieved within the first two to three weeks.
Utilizing the soft liner material can also create a functional reline impression. I will keep a patient in this soft liner until healing is complete and I am ready to have a hard acrylic lab reline performed. These materials will “bond” well enough to the denture base; I will describe later how I trim the material and get it to adhere to the borders.
The silicone elastomers are usually used for extended periods (one year). I will try this liner if a patient presents with thin, atrophied ridges, undercuts, non-resilient mucosa, or chronic soreness. It will provide a softer base than the existing intaglio, but its properties won’t change as quickly as the acrylic resin liners. This material is denser and doesn’t have the pockets of water, which form when the plasticizers leach out of the acrylic-based ones. If the patient is considering having a new denture made but is unhappy with the fit of their existing one, I will use a silicone elastomer material. It will render comfort and buy the patient time before investing in a new denture. Additionally, it may be more suitable biologically when placed over cells in recent surgical sites.1
The problem with this material is establishing a strong bond to the denture base. Mechanical retention can be cut in (I will place V-shaped undercuts where I can), and solvent-based primers are added to the denture’s intaglio to help rectify this problem. That being said, patients will always show you where it’s peeling away.
Given enough time, both types of liners will become hard and probably uncomfortable. The surface will become rough and irritating and start to peel away from the denture borders. It can also become colonized with Candida and other microorganisms, leading to chronic tissue inflammation.
Denture Liner Adhesion
Good adhesion of the liner to the denture base enhances its long-term performance. One study showed that the adhesive values obtained with a roughened surface are approximately double those of the smooth surface.
It’s worth the time spent to do this.
Altering the surface of the acrylic resin denture base by running an acrylic bur over the intaglio and borders, micro etching, applying 36 percent phosphoric acid, and utilizing the manufacturer’s recommended bonding agents should provide an adequate roughened surface. Once the surface for bonding of the liner is addressed, attention must be paid to the thinness of the material, as the thinnest areas will peel away first. In my experience, this happens often in the retromolar pad area and the posterior maxillary border. Make sure to relieve these areas 1-2 mm before applying the liner so that there is sufficient bulk and thickness.
Dentists frequently control the powder/liquid ratio of the mix to improve the handling properties and working time. Many increase the liquid to change the flow of the material. Changing the P/L ratio can create a greater plasticization effect, so follow the manufacturer’s recommended values for powder/liquid ratios.
Sealers placed on the cured liner material will act as a mechanical barrier to control the food deposits and chemicals attracted to it. Using a sealer will reduce the surface breakdown, which will occur with routine mechanical cleaning. It will also protect the incorporation of pigments (coffee, tea, wine, tobacco, etc.) into the material. Or silicone-based liner.2 Surface roughness is inevitable with either.
Cleaning Soft-Tissue Liners
Patients will ask how best to clean the dentures once the liner is placed. Peroxide-based denture cleansers are the most commonly used. They are dispensed in powders or tablets and become alkaline hydrogen peroxide solutions when dissolved in water. There has been a prevailing thought that denture cleanser use can damage the resiliency of the liners. One study looked at Coe Soft and Polident tablets and found that although there was a change in the weight of the resilient liner, the surface roughness and bond strengths were unaffected.3 The use of conventional denture cleansing tablets or a dilute mix of water with 0.5 percent sodium hypochlorite will be equally effective for either type of liner. Silicone-based liners show better compatibility and resiliency over the long term; however, the results are clinically insignificant.
If using an acrylic-based liner, I instruct the patients to initially rinse it with cold water and use a Q-tip to remove any food debris until the consistency of the liner has become denser. Then, a soft brush and denture cleansing tablets can be used. I explain that the liner will have to be changed more often because of the increased hardness that will develop. A soft brush and tablets can be used from the onset if a silicone elastomer-based liner is used.
Many dentists struggle with how to finish trimming the excess material along the denture borders.
One simple technique is to heat a #7 wax spatula with a torch or Bunsen burner and hold it perpendicular to the border.

Once in contact with the liner and denture acrylic, you can move the instrument along the outside periphery of the border. It will trim the excess without pulling it off and seal the material to the acrylic.


You don’t need to polish it anymore, as it provides a smooth and comfortable surface that will adhere to the acrylic border.


How long any one-liner will last depends on many factors, some of which are unclear. The selection of a liner cannot be based on any single property, but on the clinical situation presented. Many materials are currently available, all of which will provide the intended function. Both types of soft liners have a place in your removable prosthetic practice.
References
- Chaves, C. A., Vergani, C. E., Thomas, D., Young, A., Costa, C. A., Salih, V. M., & Machado, A. L. (2014). Biological effects of soft denture reline materials on L929 cells in vitro. Journal of Tissue Engineering, 5, 2041731414540911.
- Kutlu, I. U., Yanikoğlu, N. D., Kul, E., Duymuş, Z. Y., & Sağsöz, N. P. (2016). Effect of sealer coating and storage methods on the surface roughness of soft liners. The Journal of Prosthetic Dentistry, 115(3), 371-376.
- CM, R. (2003). Effect of a denture cleanser on weight, surface roughness, and tensile bond strength of two resilient denture liners. Journal of Prosthetic Dentistry, 29, 494-498.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Mary Anne Salcetti
Date: February 21, 2022
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


