Why Do Jaws Hurt? Rethinking Orofacial Pain in the 3D Imaging Era
We’ve all heard the question from patients: “Why does my jaw hurt?”
And if we’re being honest, most of us hesitate before answering.
Traditionally, we were taught that orofacial pain stems from hyperactive muscles and that muscle soreness usually comes from clenching and grinding under stress. But modern three-dimensional imaging has rewritten that story. With new insights into the temporomandibular joint (TMJ), we can now offer patients more accurate explanations — and better care.
Why jaw pain intimidates so many dentists
When a patient shows up with jaw joint pain, many dentists refer them to an oral surgeon, orthodontist, or “TMJ specialist.” Ironically, we handle odontogenic pain every day — some of the most intense pain a patient can experience — yet jaw joint pain makes many clinicians uncomfortable, leading them to have little to no interest in treating patients with jaw joint pain.
Why? Most dentists are intimidated to treat patients with jaw joint pain because we weren’t trained to truly understand it. Traditional education focused on muscle pain, not joint structures. Without clear visualization, we were relying on textbook sketches and best guesses.
What 3D imaging reveals about jaw pain
Enter modern imaging — CBCT and MRI. These tools have altered our understanding of the temporomandibular joint (TMJ). We now recognize that structural changes in both soft tissue and hard tissue are far more common than we thought.
Yes, muscle pain is real and often easily treatable with a properly fitted occlusal appliance. When muscle hyperactivity is the only culprit, patients can feel better fast. But when the pain lingers, it’s time to look deeper.
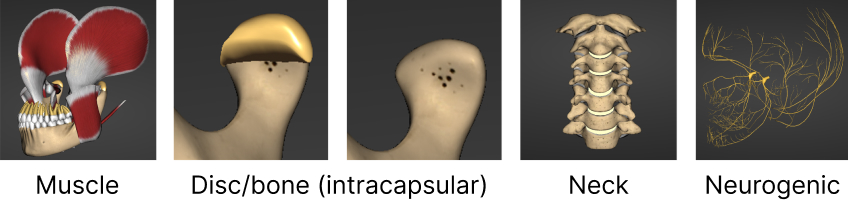
Beyond muscles: other sources of jaw pain
There may be intracapsular changes inside the TMJ, like a displaced or torn disc, or even herniation into the lateral pterygoid muscle. Hard-tissue changes are also common:
- Eroded bone, where the cortical plate of the condyle is disrupted
- Edematous bone, where internal swelling makes the area painful
- Small bone, where growth is limited after ligament injury, reducing the load-bearing surface
And let’s not forget the upper cervical spine. Misalignments within the neck are surprisingly frequent and can mimic, or even exacerbate, jaw pain. In most cases, both areas need to be addressed separately, since they follow their own paths of dysfunction.
The role of the nervous system
Sometimes, the culprit isn’t the joint or muscle at all; it’s the nervous system. Elevated sympathetic nerve activity can heighten pain sensitivity and trigger muscle dystonia, which may be a key driver of bruxism. In these cases, calming the nervous system becomes as important as adjusting the bite.
Diagnosing the true source of pain
To treat effectively, we first need to understand the source of the pain (Fig. 1). Diagnostic nerve blocks can help pinpoint the source:
- The auriculotemporal nerve block helps determine joint-related pain.
- The greater occipital nerve block identifies issues from the upper cervical spine.
- The greater auricular nerve block can reveal sympathetic system involvement.
When you combine these diagnostic tools with CBCT and MRI, you can treat patients with confidence and change lives in the process.
Take your understanding further
If you’re ready to master this level of diagnostic precision, consider joining me at the Advanced Occlusion workshop, Jan. 29–31, 2026, at Spear Campus. As the workshop presenter, I dive deep into the clinical reasoning, imaging interpretation, and hands-on skills you need to diagnose and manage complex occlusal and TMJ cases.
Your patients with jaw pain are counting on you to understand why they hurt. This is where that understanding begins.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Jim McKee
Date: December 30, 2025
Featured Digest articles
Insights and advice from Spear Faculty and industry experts



