Identifying Pulpal Necrosis for Endodontic Treatment
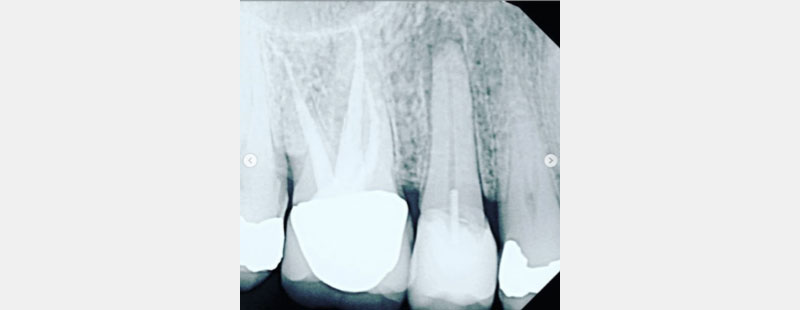
We’ve all had the same patient in the chair, whether you’re a general practitioner or an endodontist. A molar was prepped and temped uneventfully a few weeks or months ago (Figs. 1–3). The patient presents for the crown delivery appointment, and the rest can vary.

Sometimes the crown was just cemented and placed after being prepped and temped uneventfully, and the patient never reported any symptoms or discomfort (see Figs. 4–6). Often during crown treatment planning, (newer) PAs are not taken, and the crown gets prepped and temped based on the FMX from years earlier.
So, the crown was prepped and temped based on the previous year’s recent BW (often taken every two years). Unknowingly, without a “recent” PA, periapical pathology likely existed even before the crown was prepped and temporized.



Three Scenarios to Consider
Scenario 1: At cementation, the dentist notices a small draining parulis (pimple, sinus tract) and assumes periodontal involvement since the patient is asymptomatic. The dentist explains the situation to the patient, drains the abscess, adjusts the bite, writes a prescription for antibiotics, and, maybe, refers the patient to a periodontist.
Scenario 2: The patient is symptomatic after the prep and temporary appointment. They call the office to report cold-like symptoms, but when they present, the symptoms are not reproducible or remarkable. Both patient and dentist agree to go ahead and cement the crown since the symptoms come and go for the most part, but there have been fewer since the patient’s first call.
Scenario 3: The patient returns asymptomatic, and the delivery goes well. Several days/weeks/months/years later, the patient returns with either symptoms of throbbing pain or with a facial swelling and asks you how this happened.
Dentists may ask if there was anything they could have done differently. Patients often ask this of endodontists.
Each scenario could result in a different flowchart. Still, as an endodontist, my suggestion is to take a periapical film before any crown is planned, even if the crown is going to be replaced. I suggested this recently to an audience of general practitioners, and a dentist with 24 years of experience responded that they always “have a recent film of the tooth” in question. I asked that dentist to define “recent.”
Insurance guidelines suggest BW every two years and FMXs (PAs) every five years, so how recent is the “recent” PA you’re referring to? Why not take a very recent PA (within the past two months) of any tooth with a large restoration (three surfaces or more) that is about to be replaced, added to, or crowned?
A recent PA, with the BW you might already have, will provide essential information about that tooth. Are the pulp chambers uniform and evident? Can you see the pulp chambers? Are they grey? Or are they sandwiched and shrunken (aka calcifying or calcified)?
Can you cold test the tooth? If calcified, it might not respond to cold, so how do you assess? Is the cold response the same intensity as all the other teeth? Can you percuss the tooth? Is it different in how it feels versus the adjacent teeth or virgin nearby teeth (if applicable)? If not, can you suggest an endodontic consultation?
In Scenario 1, if the periodontist also does not test the tooth for pulp vitality and the true origin is endodontic in causation, misdiagnosis can continue since most endodontic symptoms resolve temporarily with antibiotics. The tooth that most likely needed endodontic therapy might unnecessarily receive periodontal therapy and/or later become a bigger problem with fewer or less optimistic treatable solutions.
In Scenario 2, the symptoms have falsely disappeared or “resolved.” However, pulpal necrosis will likely continue, and eventually, symptoms and/or an abscess/swelling may appear.
In Scenario 3, pulpal necrosis (likely present prior to crown cementation) progressed, resulting in facial swelling. However, each scenario could have likely been avoided with the suggested limited testing in conjunction with a PA film and an endodontic consultation.
As a side note, it usually takes approximately three months for radiographic changes of pulpal necrosis to become evident with a periapical lucency. Please remember these lucencies aren’t always evident.
Room for Improvement — The Year of the PA
I’m a systems-type person. I like flowcharts and checklists. These two suggestions below will decrease your post-crown cementation complications and prevent many patients from becoming disgruntled about their symptoms or having you or an endodontist create access through their beautiful and costly new crown.
In Figs. 7–9, each patient was asymptomatic, but clearly all had medium- to large-sized restorations.


Many patients present to endodontists by saying their dentist told them their (now symptomatic) tooth “might need endo” (several years ago). Why are we so timid and fearful about this critical conversation, and why are patients still so scared of endodontics?
I speak to many practitioners who still admit they cannot comfortably deliver the “you need a root canal” conversation with their patients. Let’s embrace this. Let’s step up our patient conversations and educate them so that they can avoid unnecessary pain and discomfort. Let’s script this, rehearse, and change the dialogue to make it a positive conversation — preferably in advance and possibly during the treatment planning. My first suggestion would be something like:
“Hey, Mr. Smith, this is an extensive filling. It would be best if you had a [root canal] before we place the crown (though you could also say endodontic or pulpal therapy to minimize the patient’s negative response). It would avoid potential discomfort or having to drill through the beautiful new crown after it’s placed. I know it’s not what you might want to hear, but it would save you time, money, and discomfort in the long run.”
If the patient wants to hear a bit more about the biology and why, feel free to elaborate. To patients with and without symptoms, I explain:
“The nerve inside the teeth is very delicate; unfortunately, the nerve tissue does not like cavities or fillings getting too close to it. Over time (or suddenly), we have gotten too close to the nerve tissue, which will likely be harmed. Unlike the rest of your body, it won’t be able to recover or heal itself, and that is why endodontics is indicated. I want to offer to have it done sooner to avoid the symptoms, discomfort, or ruined weekend or holiday, since it can surprise you anytime and even land you in the emergency room.”
Some patients will opt to gamble. But knowing this, I’d like to think you’ll get more “takers.”
I suggest introducing your patient to your endodontist via an in-office tablet or pamphlet if that’s easier. Confirming that the specialist you’re referring them to is an experienced clinician with a thriving practice is essential. Introducing your patient to your endodontist and their team is highly comforting to patients. Otherwise, they will most likely fold up your referral slip, wait for symptoms, and default to one of the scenarios above.
I also ask that you educate your front desk and other team members. If you are inclined, could you ask your endodontist about key phrases to listen for when patients call to report pain? With this awareness, your office and the patient will be relieved to avoid wasted time and resources. Would you and your staff like the patient to go directly to the endodontist? Decide as a team and embrace this new system. If anything, try it out for a few months.
Likewise, dental hygienists should also be empowered since they often have the closest relationships with the patients. Have every hygienist ask patients about dental discomfort or pain during each visit. Have them selectively take PA films on heavily restored teeth. When they probe, if there are isolated pockets, purulence, or a sinus tract, be sure to take a PA film and have them notify you. This is an important indicator of potential/likely endodontic disease.
Many dentists tell me, “I told the patient they needed (endo).” With confidence and rephrasing, endodontics doesn’t have to be so negative, and your patients will better grasp how endodontics helps save teeth and eliminate pain.
References
- Berman, L. H., & Hargreaves, K. M. (2015). Cohen’s Pathways of the Pulp Expert Consult. Elsevier Health Sciences.
- Sigurdsson, A. (2003). Pulpal diagnosis. Endodontic Topics, 5(1), 12-25.
- Huumonen, S., & Ørstavik, D. (2002). Radiological aspects of apical periodontitis. Endodontic Topics, 1(1), 3-25.
VIRTUAL SEMINARS
The Campus CE Experience
– Online, Anywhere
Spear Virtual Seminars give you versatility to refine your clinical skills following the same lessons that you would at the Spear Campus in Scottsdale — but from anywhere, as a safe online alternative to large-attendance campus events. Ask an advisor how your practice can take advantage of this new CE option.

By: Judy McIntyre
Date: February 19, 2020
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


