Internal Bleaching of the Dark Tooth
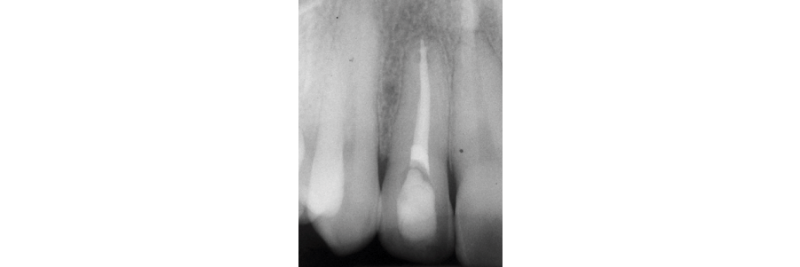
One of the most challenging clinical situations encountered in practice is restoring a “dark tooth” in the esthetic zone (Figs. 1A, 1B).

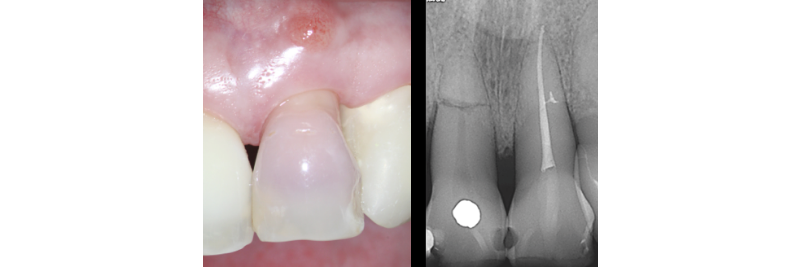
One treatment option that is often overlooked is internal non-vital tooth bleaching. This can be an excellent treatment option if the tooth has had RCT or needs RCT (Figs. 2A, 2B).


This treatment option is not often recommended because most dentists were taught that internal non-vital tooth bleaching has a high risk of creating internal/external resorption. While this was true in the past, with the changes in material (sodium perborate instead of hydrogen peroxide) and technique (walking bleach instead of heated bleach), the risks are now quite low.
The technique for “walking bleach” is outlined as:
- Leave gutta percha 1.0–2.0 mm below the CEJ
- Place a “base” to seal the gutta-percha
- Place sodium perborate in access against the barrier and seal
- Replace material as necessary to obtain desired change
- Wait 15 days before placing definitive composite restoration to close access (to obtain optimal bond strengths)
Predictability and Stability
Abbott (2009) evaluated 225 teeth treated with internal bleaching and assessed color modification as “good” in 87.1% of the teeth and “fair” in 12.9% of the teeth.
Dark yellow and black teeth were less predictable (requiring more applications) than light yellow and grey teeth. Amato (2006) published a 16-year follow-up on 50 teeth treated with internal bleaching and reported that in 62.9% of the teeth, the color had remained stable, while there was a marked color change in 37.1%.
Additionally, none of the teeth in this study had any signs of internal or external resorption at 16 years. A more recent paper (Amato, 2018) reported 85% of the teeth treated with internal bleaching had color stability at 25 years.
It must be stated that ample access preparation (Figs. 2A, 2B) is not required to internally bleach non-vital teeth, as a larger access preparation further compromises the tooth structurally. Figures 3A and 3B illustrate successful outcomes with a much more conservative approach (treatment by Dr. Steve Baerg, Gig Harbor, Washington).

So, the next time you come across a dark tooth in the esthetic zone, ask yourself if internal bleaching is a possible treatment solution before you pick up the handpiece.
References
- Abbott, P., & Heah, S. Y. S. (2009). Internal bleaching of teeth: an analysis of 255 teeth. Australian Dental Journal, 54(4), 326-333.
- Amato, M., Scaravilli, M. S., Farella, M., & Riccitiello, F. (2006). Bleaching teeth treated endodontically: long-term evaluation of a case series. Journal of Endodontics, 32(4), 376-378.
- Amato, A., Caggiano, M., Pantaleo, G., & Amato, M. (2018). In-office and walking bleach dental treatments on endodontically-treated teeth: 25 years follow-up. Minerva Stomatol, 67(6), 225-30.
VIRTUAL SEMINARS
The Campus CE Experience
– Online, Anywhere
Spear Virtual Seminars give you versatility to refine your clinical skills following the same lessons that you would at the Spear Campus in Scottsdale — but from anywhere, as a safe online alternative to large-attendance campus events. Ask an advisor how your practice can take advantage of this new CE option.

By: Greggory Kinzer
Date: October 7, 2019
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


