Should I Be Thinking About TM Imaging?
Temporomandibular imaging allows us to gain insights into the anatomy of the TMJ. While TMJ imaging was once rare, it is now commonplace for dentists to image the TMJs. Since it is impractical to obtain TM imaging for every patient, we need guidelines on when to do so. When we decide to obtain TM imaging, the best option is to perform soft tissue imaging with MRI and hard tissue imaging with CBCT.

Recognizing patients who need TM imaging
When considering whom to image, an easy way to identify patients who could benefit from imaging is by addressing two questions: How do the patient’s teeth fit in the skeletal position, and does the patient experience regular pain?
Assessing skeletal position to identify indicators for TM imaging
The first question is how the teeth fit in a skeletal position? If there is a Class II occlusion in a fully seated condylar position, it may be a good idea to obtain TMJ imaging.
As Manfredini (2016) wrote, “It seems reasonable to suggest that skeletal Class II profiles and hyperdivergent growth patterns are likely associated with an increased frequency of TMJ disc displacement and degenerative disorders.”
Patients who present with Class II occlusions, high mandibular plane angles, anterior open bites, canted occlusal planes, deep bites, overjets, facial asymmetries, and retrognathia all have an increased likelihood of having structurally altered TMJs. If we can recognize these patients and obtain MRI/CBCT imaging, we will have increased confidence when treatment planning and increase case acceptance.
Assessing the frequency of patient pain
The second question to consider when determining whether patients could benefit from TMJ imaging is whether they experience regular pain. While the frequency of pain is usually discussed, it is also helpful to assess the severity of the pain when determining if TMJ imaging may be helpful.
We were taught that the majority of pain results from muscle hyperactivity; today, we know that changes in the condition and position of both the disk and the condyle can have a significant impact on pain levels. Generally, if patients report pain levels greater than five on a 1-10 scale, it may be beneficial to obtain MRI and CBCT imaging to understand the anatomical risk factors better.
Understanding TMJ classification in clinical practice
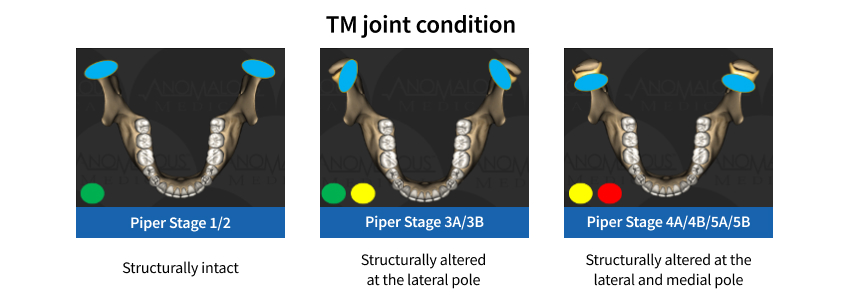
When considering the various types of joints observed in clinical practice (Fig. 1), most patients can be categorized into one of three groups: structurally intact TMJs have normal joint anatomy. Structurally altered TMJs at the lateral pole have an intact disc at the medial pole and a displaced disc at the lateral pole. Structurally altered TMJs at the lateral and medial poles have a displaced disc at both locations.
Since the medial pole is the load-bearing portion of the TMJ, if the disc does not protect the medial pole, it becomes more difficult to dissipate the daily loading forces. This increases the likelihood that the patient will report pain. Additionally, the disc at the medial pole acts as a three-dimensional gasket to maintain the vertical dimension in the TMJ. If the disc is herniated and cannot maintain the TMJ’s vertical dimension, it increases the likelihood that the patient will have a Class II bite shift.
In summary, an easy way to decide if a patient should obtain TM imaging with MRI and CBCT is to ask yourself two questions:
- Does the patient have pain greater than five on a 1-10 scale?
- Are the teeth uncoupled greater than the thickness of the disc?
If the answer to either or both questions is yes, consider the soft and hard tissue in the TMJ to increase your confidence in diagnosing and treating TMJ patients. Once you begin imaging TMJs, be prepared for an increase in the number of new patients. There are patients in your community seeking a TMJ diagnosis, and there are dentists in your community looking to refer patients to someone who can recognize, diagnose, and treat these conditions.
References
- Manfredini, D., Segù, M., Arveda, N., Lombardo, L., Siciliani, G., Rossi, A., & Guarda-Nardini, L. (2016). Temporomandibular joint disorders in patients with different facial morphology. A systematic review of the literature. Journal of Oral and Maxillofacial Surgery, 74(1), 29-46.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Jim McKee
Date: July 18, 2024
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


