Integrating Myofunctional Therapy Training into Your Dental Practice with BROOM Screening
Editor’s Note: This article was written jointly by Brittny Sciarra, RDH, and Karese Laguerre, CRDH
In 2017, the ADA released a policy statement encouraging dental professionals to screen for red flags that may indicate a possible airway obstruction. Dental hygienists play a crucial role in screening patients for sleep-related breathing disorders. These disorders can range from mouth breathing to snoring, upper airway resistance, and obstructive sleep apnea. In this article, we will be discussing myofunctional therapy training for dental staff using a screening tool referred to as “BROOM.”

Myofunctional therapy training using BROOM screening
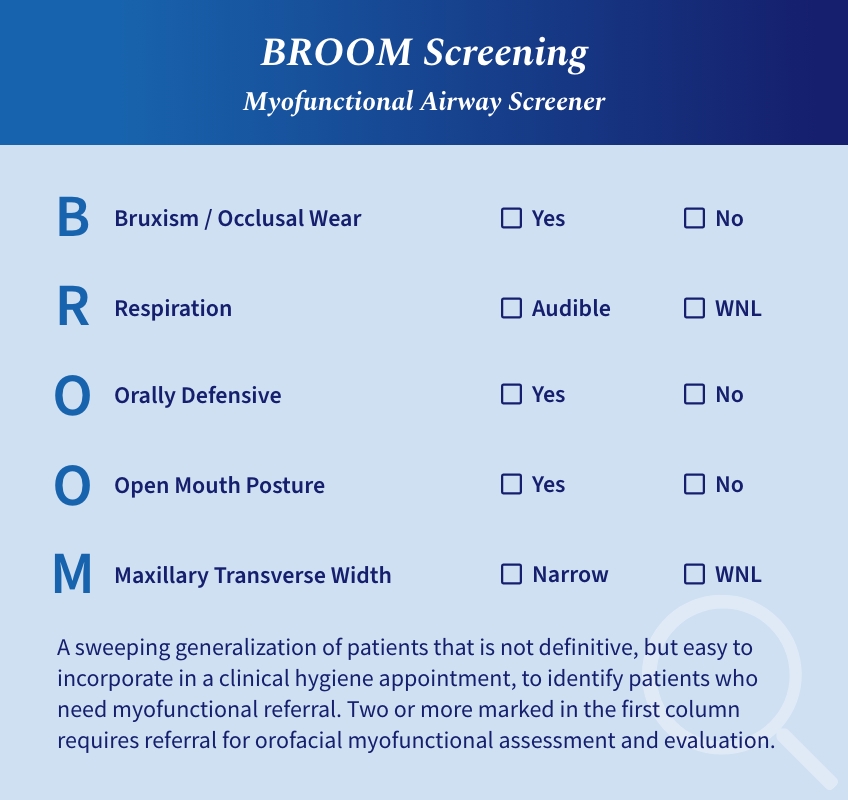
BROOM is a sweeping generalization used to identify patients who need a myofunctional therapy referral. While not definitive, it can be easily incorporated into a clinical hygiene appointment and completed by the time you finish your intraoral and extraoral examinations. The BROOM screening consists of five parts:
- B: Bruxism / Occlusal Wear
- R: Respiration
- O: Orally Defensive
- O: Open Mouth Posture
- M: Maxillary Transverse Width
B: Bruxism/occlusal wear
Patients who come in with complaints of tenderness in the muscles of mastication and are showing occlusal wear are generally recommended a traditional night guard. Many airway focused dental providers no longer utilize traditional night guards in their armamentarium. By conducting myofunctional therapy training with your staff, the patient who is showing signs of occlusal wear may be a candidate for referral. Checking for bruxism or occlusal wear is the first step in BROOM screening.
According to sleep medicine specialist Dr. Jerald Simmons, MD and sleep dental specialist Dr. Ronald Prehn, DDS, “when most patients exhibit obstructive respirations during sleep the mandible falls back bringing the back of the tongue with it. This triggers a series of events that in some people results in a reflexive attempt to open the airway by increasing masseter tone. This brings the mandible forward and, in many patients, improves respirations. We postulate [sic] that nocturnal bruxism is a compensatory mechanism of the upper airway to help overcome upper airway obstruction by activation of the clenching muscles which results in bringing the mandible, and therefore the tongue, forward.”1
Myofunctional therapy can aid in the patency of the upper airway. According to Guimar in 2018, “oropharyngeal exercises significantly reduce OSAS (obstructive sleep apnea syndrome) severity and symptoms and represent a promising treatment for moderate OSAS.2 A clinical study conducted by Messina in 2017, documents the benefits of myofunctional therapy on bruxism. This study showed that myofunctional therapy can be “an effective therapeutic strategy regarding the treatment of muscle facial pain and hypertonia of the chewing and swallowing muscles. All treated patients had a reduction of facial pain and a reduction in the number of bruxism episodes per hour, and in many cases, such episodes disappeared.”3 Another indication to look for intra-orally is the presence of maxillary or mandibular tori. According to research, tori are associated with the presence of abnormal tooth wear due to the abnormal pressure on the teeth.4
R: Respiration
Next check your patient’s breathing by observing your patient in their most natural state while they are sitting in your dental chair.
- Are they breathing through their nose or their mouth?
- Do their breaths seem to be coming primarily from the chest or from the diaphragm?
- Are their breaths shallow?
- Are they audible?
Dominant mouth-breathing patterns can alter the development of the craniofacial complex and may cause relapse in orthodontic retention. According to Zhao in 2021, mouth breathing affected facial skeletal development and malocclusion in children. “The mandible and maxilla rotated backward and downward, and the occlusal plane was steep. In addition, mouth breathing presented a tendency of labial inclination of the upper anterior teeth.”5
In 1907, Dr. Edward Angle published Malocclusion of the Teeth, in which he recognized the influence of mouth breathing on oral rest posture and successful orthodontic treatment.6 Optimal oral rest posture includes the entire tongue resting on the roof of the mouth, lips closed, and dominant nasal breathing. This posture should be maintained while awake and asleep. Correct oral rest posture is the goal of myofunctional therapy training, and therefore, should always be included in a patient’s treatment plan who does not exhibit dominant nasal breathing patterns.
O: Orally defensive
Many scenarios can lead to a positive answer to the next step in the BROOM screening. Can you think of a patient whose tongue is constantly battling you, or a patient whose lips are so tense you can hardly retract? How about fighting the lower lip to scale the mandibular anterior dentition? What if we told you that a gag reflex can be a patient’s response to protect their own airway? The scenarios above may all be a sign of orofacial dysfunction and indicate the need for further myofunctional evaluation.
Patients with increased vertical growth tend to have an overactive mentalis muscle. Think of those patients with gummy smiles or retrognathic mandibles. An overdeveloped mentalis muscle may also form by serving as a compensatory pattern to keep the lips closed.
Lingual control and optimal lingual function play a crucial role in optimal craniofacial growth and development, mastication, swallowing, speaking, and keeping the upper airway open during sleep. Myofunctional therapy includes exercises to strengthen the tongue and orofacial muscles. Oropharyngeal exercises effectively modify tongue tone.7
O: Open mouth posture
Open mouth posture can also be a sign of airway obstruction. By observing your patient, you may be able to see some of these signs.
- Are their lips together or apart?
- Where are their lips when you call their name, or when they sit in your dental chair?
- When you’re speaking to them, how are they posturing their lips?
- Do they have a flaccid, or rolled out, lower lip?
- Are their lips dried or cracked?
- Are they applying Chapstick while in the dental operatory?
If you do see signs of open mouth posture, it is imperative to work collaboratively with an otolaryngologist, or ENT, to evaluate for nasal patency. It can be indicative of allergies, enlarged tonsils and/or adenoids, enlarged nasal turbinates, nasal polyps, or a deviated septum and can lead to improper tongue posture, reverse swallowing pattern, and/or malocclusion. Conducting myofunctional therapy training ensures that these patients will get the extra treatment that they need.
M: Maxillary transverse width
Does your patient present with crowding? This is the final sign that your patient may benefit from myofunctional therapy. When measuring the maxillary transverse width, we measure from tooth #3 to #14 on the maxillary arch. Dr. James A. McNamara provides a range of 36 to 39 mm, indicating that the maxillary arch can accommodate a dentition without crowding or spacing.8 The simplest and quickest thing to do is to take a cotton roll and measure it with your periodontal probe. Cotton rolls are generally about 36-37 mm.
The maxilla also makes up the floor and lateral walls of the nasal cavity. Generally, the size of the maxilla mirrors the size of the nasal cavity. If the maxilla develops narrowly, we often have an insufficient oropharyngeal space. When addressing the root cause of underdeveloped jaws, we must not ignore tongue rest posture. The tongue should live in the roof of the mouth. An analogy we have heard from Dr. Ben Miraglia speaks to this: “Your tongue should fit in the roof of your mouth, like your car fits in your garage”. In utero, the tongue begins to shape the structure of our jaws and nasal airway. The tongue pushes the palate forward and to the sides. It is the counterbalancing forces that allow our arches to reach their fullest potential and develop proper bone growth. The tongue is the architect, creating a scaffold for the development of a U-shaped arch that can accommodate all thirty-two teeth.
Referring your patient
Conducting myofunctional therapy training for dental staff using a screening tool referred to as BROOM provides essential details about your patient’s overall health. After reviewing the BROOM checklist, if two or more signs are present, the patient should be referred for an orofacial myofunctional assessment and evaluation.
References
- McNamaraa, J. A. (2000). Maxillary transverse deficiency. American Journal of Orthodontics and Dentofacial Orthopedics, 117(5), 567-570.
- Simmons, J. H., & Prehn, R. S. (2008). Nocturnal bruxism as a protective mechanism against obstructive breathing during sleep. Sleep, 31(Suppl 1), A199.
- Guimarães, K. C., Drager, L. F., Genta, P. R., Marcondes, B. F., & Lorenzi-Filho, G. (2009). Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. American Journal of Respiratory and Critical Care Medicine, 179(10), 962-966.
- Guimarães, K. C., Drager, L. F., Genta, P. R., Marcondes, B. F., & Lorenzi-Filho, G. (2009). Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. American Journal of Respiratory and Critical Care Medicine, 179(10), 962-966.
- Messina, G., Martines, F., Thomas, E., Salvago, P., Fabris, G. B. M., Poli, L., & Iovane, A. (2017). Treatment of chronic pain associated with bruxism through Myofunctional therapy. European Journal of Translational Myology, 27(3), 6759.
- Bertazzo-Silveira, E., Stuginski-Barbosa, J., Porporatti, A. L., Dick, B., Flores-Mir, C., Manfredini, D., & De Luca Canto, G. (2017). Association between signs and symptoms of bruxism and presence of tori: a systematic review. Clinical Oral Investigations, 21(9), 2789-2799.
- Zhao, Z., Zheng, L., Huang, X., Li, C., Liu, J., & Hu, Y. (2021). Effects of mouth breathing on facial skeletal development in children: a systematic review and meta-analysis. BMC oral health, 21(1), 108.
- Paul, J. L., & Nanda, R. S. (1973). Effect of mouth breathing on dental occlusion. The Angle Orthodontist, 43(2), 201-206.
- Villa, M. P., Evangelisti, M., Martella, S., Barreto, M., & Del Pozzo, M. (2017). Can myofunctional therapy increase tongue tone and reduce symptoms in children with sleep-disordered breathing?. Sleep and Breathing, 21(4), 1025-1032.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Brittny Sciarra
Date: June 23, 2022
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


