Oh Snap! Managing a Fractured Denture Base
Any time a prosthesis is removable by the patient, one of the risks dentists and their patients need to be aware of is damage to the prosthesis from being dropped.
Dropping a removable prosthesis may result in chipped or broken teeth, but it often results in a fractured denture base. While dropping the prosthesis is a common cause of fractured denture bases, it is not the only cause. As a patient’s arches resorb, it is not uncommon to see denture bases fracture due to stress concentrating in areas that haven’t resorbed — the maxillary mid-palatal suture, for example.
As a result, fractured denture bases are common with this group of patients, and regardless of the cause, a fractured denture base can be an urgent concern for the patient. In many cases, the damaged prosthesis can be sent to the dental laboratory for repair, but what if the lab isn’t available? In this article, I want to share a case presentation for a patient in just this predicament.
Initial Situation
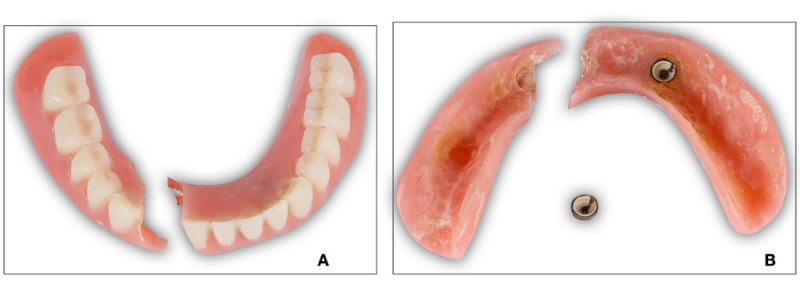
A 91-year-old female in good general health was referred for urgent repair of her lower denture. The patient had implants placed and both arches restored with implant-retained overdentures about seven years before this appointment. She is unsure about the last time she had the prostheses evaluated or adjusted. She notes they are “fitting loose.” Additionally, the patient reports two previous attempts by another dentist to repair the broken denture (Fig. 1). When asked what she was doing when the denture broke? She is unsure and/or can’t remember. Upon inspection, the mandibular prosthesis is a two-implant overdenture that has fractured right through the area of one of the attachment housings.
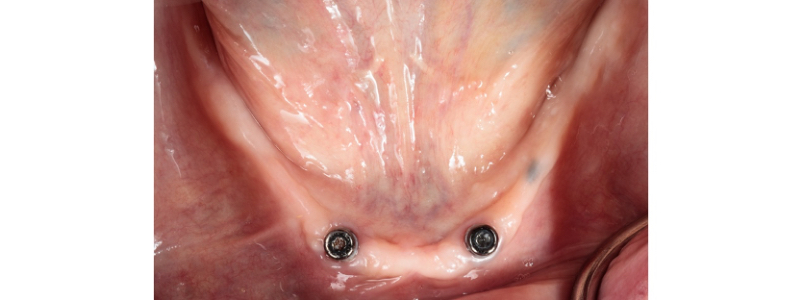
Clinically, the mandibular arch is significantly resorbed, and two implant abutments are present, but the surface appears worn. While you may not recognize these abutments, the design concept with the mandibular prosthesis is the same as a two-implant locator overdenture (Fig. 2).
According to the patient and the referring dentist, the upper and lower arches were treated approximately seven years prior. Additionally, the patient confesses to wearing both dentures at night to help prevent wrinkles from forming. In the maxilla, two abutments similar to the mandibular abutments are present in the anterior region, while the posterior two abutments appear to be angle-corrected and custom-fabricated Locators (Fig. 3). Despite the age of the case and the damage to the lower prosthesis, the maxillary prosthesis has managed to maintain its esthetics (Fig. 4). Neither prosthesis has any metal reinforcement.


Looking occlusally at the maxillary prosthesis, significant wear to the denture teeth is present. At seven years, this finding is not unexpected for conventional dentures and is indeed expected with implant-retained overdentures. Interestingly, the maxillary overdenture lost one of the retentive elements entirely, and the remaining three retentive clips do not provide much retentive value (Figs. 5 and 6).


Treatment Planning
From a treatment planning perspective, this patient presents with two challenges. The first challenge is managing the urgent problem of the fractured denture base. The second challenge is determining options for her definitive care. Understandably, additional information will be required to develop the definitive plan, but the patient is unwilling to go without a lower prosthesis while that plan is developed. To move forward, the patient needs to know that the repair to the lower overdenture will leave the denture weaker than it was initially, and any factors that contributed to the denture base fracturing, such as stress concentration around the implant abutments, could compromise the weakened denture further.
Prosthetic Procedures
In this case, the patient strongly desires to have the lower denture repaired. This particular repair has two distinct parts: part one is to repair the fractured denture base, and part two is to connect the attachment to the repaired denture base. The first step is to accurately reposition the denture base fragments (Figs. 7 and 8). This step is critical, as an error here could create problems with the fit of the denture base to the ridge and occlusal discrepancies.


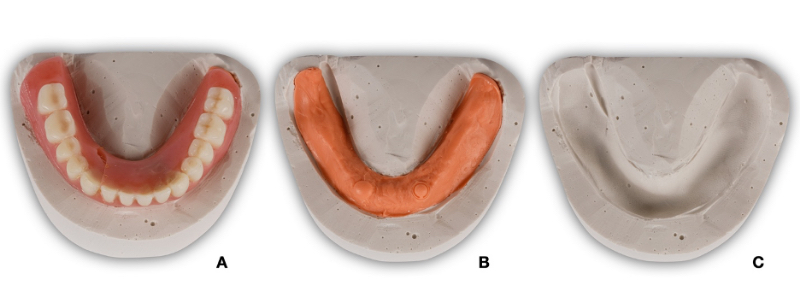
The next step is to fabricate a matrix to maintain the orientation of the fragments while the repair is being made. A remount cast is fabricated (Figs. 9 and 10).

After the remount cast is fabricated, the mandibular prosthesis is carefully removed, and the surface is prepared for the repair material. In this case, the repair material selected is an autopolymerizing acrylic resin (Jet Acrylic, Lang), so the surface is roughened with a carbide bur and air abraded with 50 micron particles of aluminum oxide (Figs. 11–3).

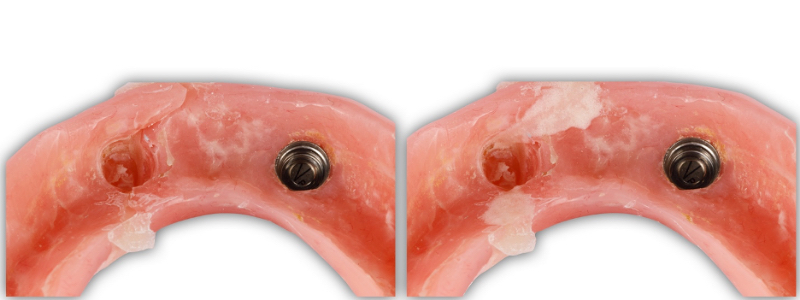

With the denture base repaired, part two of the procedure — the chairside pick-up — is ready to begin (Figs. 14 and 15).


Final Result
The prosthesis is finished with carbide burs and polished using pumice flour and denture polish on a rag wheel and lathe (Fig. 16). Alternatively, a silicone polishing system could have been utilized. The final result is then inserted (Fig. 17).


Conclusion
Denture base fracture is not uncommon in practices that treat edentulous patients. While sending the prosthesis to the dental laboratory for repair is often a great option, there may be clinical circumstances that won’t allow that to occur in a timely manner. I’ve demonstrated one way to solve this problem in this article, but there are countless other variations. I hope this helps next time you encounter this clinical problem.
References
- Abushowmi, T. H., AlZaher, Z. A., Almaskin, D. F., Qaw, M. S., Abualsaud, R., Akhtar, S., … & Baba, N. Z. (2020). Comparative effect of glass fiber and nano‐filler addition on denture repair strength. Journal of Prosthodontics, 29(3), 261-268.
- Gad, M. M., Rahoma, A., Abualsaud, R., Al‐Thobity, A. M., & Fouda, S. M. (2019). Effect of repair gap width on the strength of denture repair: an in vitro comparative study. Journal of Prosthodontics, 28(6), 684-691.
- Deb, S., Muniswamy, L., Thota, L., Swarnakar, A., Deepak, P. V., & Badiyani, B. K. (2020). Impact of surface treatment with different repair acrylic resin on the flexural strength of denture base resin: an in vitro study. The Journal of Contemporary Dental Practice, 21, 1137-1140.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Darin Dichter
Date: May 26, 2021
Featured Digest articles
Insights and advice from Spear Faculty and industry experts



