The ‘Wizardry’ of Light-Curing Adhesive Resin

(Both photos via Shutterstock.)
“The wand chooses the wizard. That much has always been clear to those of us who have studied wand lore. These connections are complex. An initial attraction, and then a mutual quest for experience, the wand learning from the wizard, the wizard for the wand.”
That quote is from Garrick Oliver, who in the Harry Potter series is the proprietor of the best wandmaker in the world. How can this “wand” reference also relate to adhesive resins?
Resin-based restorative materials are essential to contemporary esthetic restorative dentistry, and using them with confidence and predictability is instrumental to successful outcomes. The light-curing device is the quintessential “wand” for incorporating predictable resin adhesion into practice and creating magical outcomes. So, the dentist who understands and effectively applies light-curing concepts and processes is truly a restorative wizard.
This article outlines important concepts and implications related to light-curing resin materials. No matter the mode of activation (light-cure vs. self-cure), knowing the basic events that occur during the polymerization process will help dentists make the right adhesive decisions and control the outcomes.
“Harry was able to perform extraordinary feats with his wand.”
Most resin-based restorative products use the same basic monomer family and involve a polymerization mechanism. It’s essential to understand how this process works to have predictability in the process and outcome.
Methacrylates make up the basic structure of resin-based materials. The carbon-to-carbon bond is the backbone of these monomers and the starting point for polymerization, because it’s an electron-rich bond. This bond is called the vinyl group, and the methyl group is bonded to the alpha carbon. The methacrylate structure is illustrated in Fig. 2, where the “R” symbol represents various substitution groups that can be added to create unique chemical and adhesive properties.
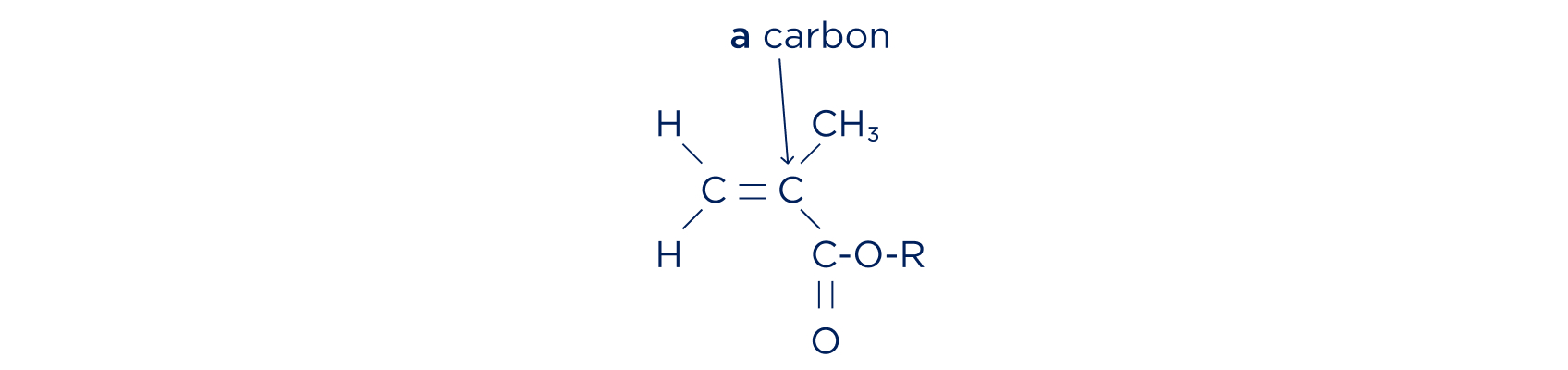
Polymerization involves the creation of free radicals. The vinyl group can be thought of as a compressed spring awaiting the release of the constrained energy. When activated through radiant (light), chemical (self-cure), or thermal energy, this bond is broken and free radicals form. These free radicals react with other vinyl groups to link together (polymerize) other methacrylate groups, thus forming a polymer chain.
Formation of free radicals and the degree of polymerization are related to the intensity of energy supplied and the amount of monomer present. The polymerization process ends when the free radicals are eliminated and the polymer chain (connection/adhesion) is completed. Creating these polymerized resins is the “extraordinary feat” behind the esthetic dentistry possible through these chemical reaction processes.
“Harry’s wand contained a phoenix feather core along with holly wood. Nothing will stand in the way of this unusual pairing of core and wand wood with its rightful match.”
Resin curing requires an initiating reaction.
For self-cured materials, the reaction between chemical ingredients launches the polymerization process. The proper mixture of chemical initiators is responsible for adequate and complete polymerization.
In the case of light curing, the free-radical initiation occurs from activation of photo initiators within the resin matrix. These photo-responsive chemicals begin the polymerization through absorbing light of various wavelengths.
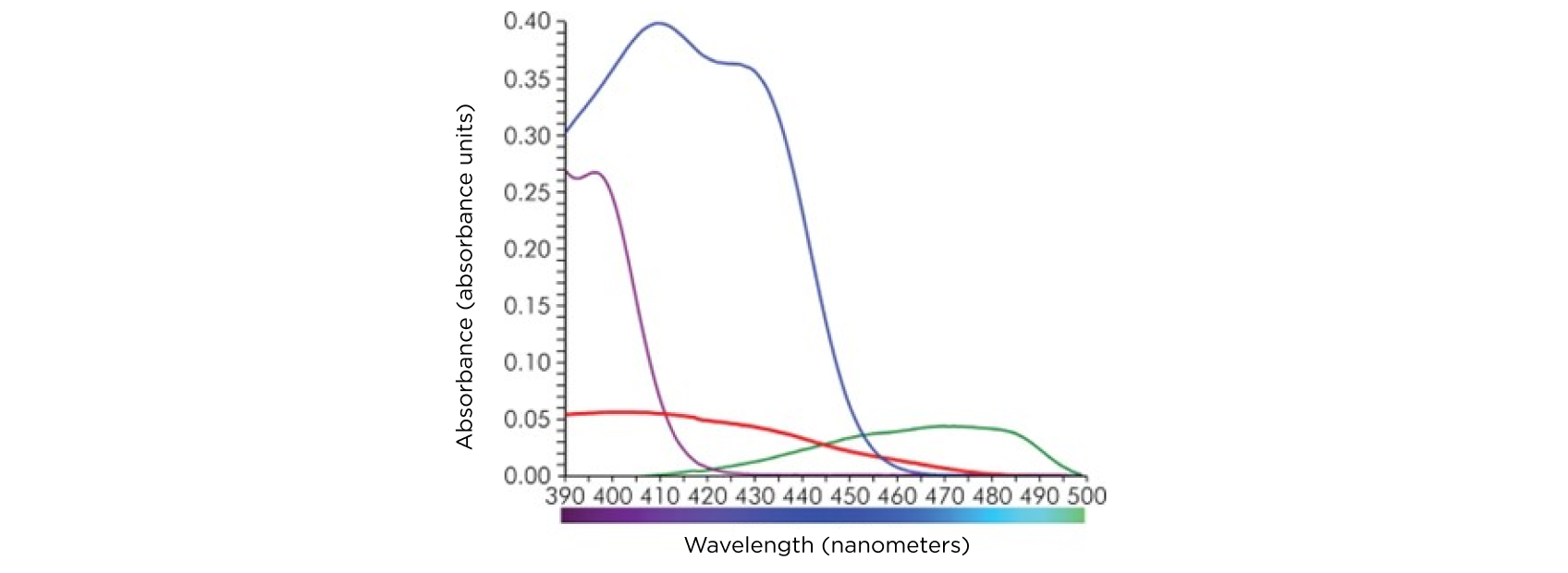
The most common photo initiator is camphorquinone. This, like phenylpropanedione (PPD), is a Type II initiator in that it requires reaction with a chemical amine to produce free radical activation. Type I initiators, such as Lucirin TPO or Ivoclar Ivocerin, have intrinsically high absorbance and more efficient quantum yield in comparison with Type II initiators.
Resin photoinitiations are activated within the visible light spectrum (400–700 nanometers). All respond to the blue or violet spectral wavelength range, but each has its own absorbance quality or level (Fig. 3).
“Various wands created differing performance qualities and outcomes.”
The first visible-light-polymerized direct composite was placed in 1976, with tungsten filament as the light source. Since then, many light sources and variations have been developed.
The development of LED technology revolutionized light activation. Unlike previous sources that required filament activation and optical filters, LED devices have reduced power requirements, can be battery-powered, and have increased photon-generating capabilities to initiate light-cured polymerization.
Initially, LED sources were large in dimension and created significant heat; gun-like devices were common because the larger bodies that held the light sources were used to dissipate the heat. As LED technology progressed, diodes became smaller and more powerful yet produced minimal heat intensity. Although gun-style LED lights are still available, pencil-style lights are standard today because their diodes are at or near the emitting end of the light wand, which helps direct the light parallel to the source, creating ease of intraoral placement and transfer of direct illumination to the resin or adhesive.1
“He wielded his wand in many epic conflicts.”
Much of the dentistry performed today depends on resin polymerization, so the indications for light-activated restorative procedures are the mainstay of corrective and therapeutic practice. However, many dentists take light curing for granted. The literature is filled with descriptions and evaluations from general practices that report their curing units deliver inadequate light output. Most curing units are also poorly maintained or cared for. These are disastrous findings, given the importance and magnitude of managing the proper light output critical to long-term restoration success.
Manufacturers typically measure irradiance at the tip of the light source, so dentists who look at those values alone may believe they’re using a powerful light source. However, significantly reduced irradiance may be reaching the resin surface, which is often 2–8 millimeters away from the end of the curing tip (Fig. 4). Some curing lights deliver less than 25% of irradiance at 8 mm2!
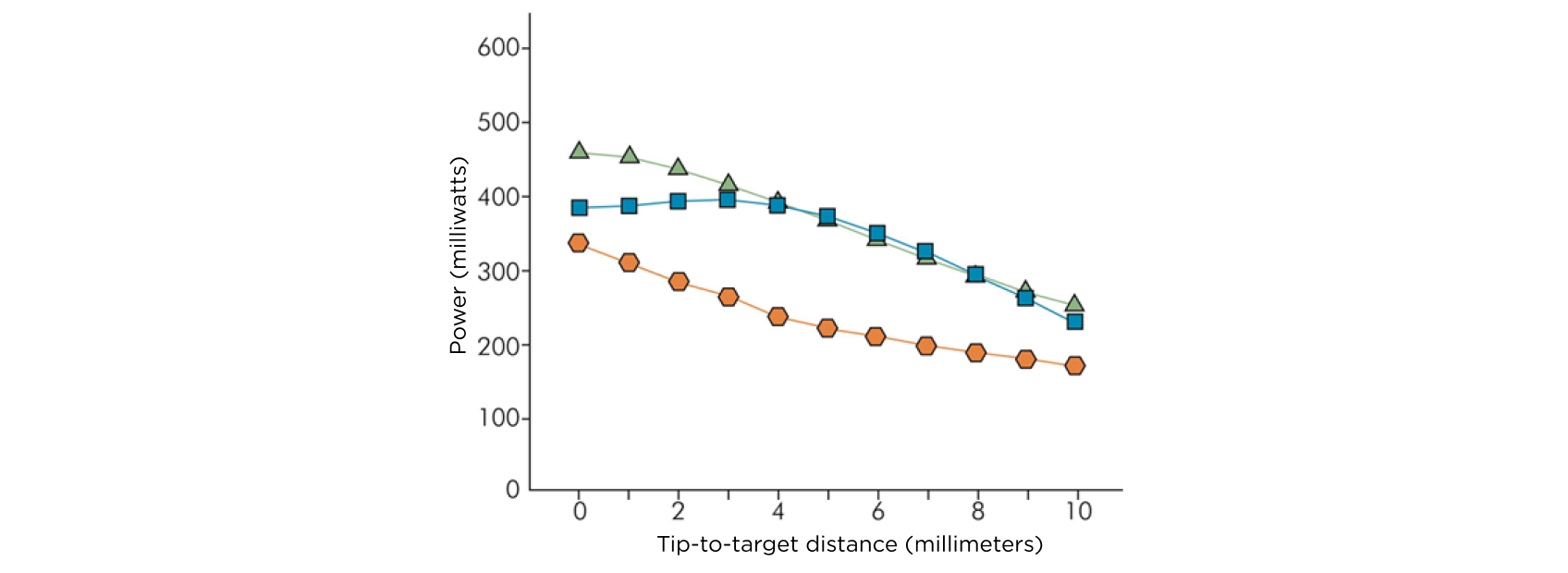
Dentists need to account for depth and distance when curing resin materials. This information becomes highly relevant at the gingival margins. Inadequate polymerization at gingival marginal locations results in marginal staining, secondary caries and early failure of the restoration. Longer curing times may be appropriate with increased depth or distance from the light source.3
“Harry possessed the magical knowledge and experience that could be said to significantly exceed that of his fellow students.”
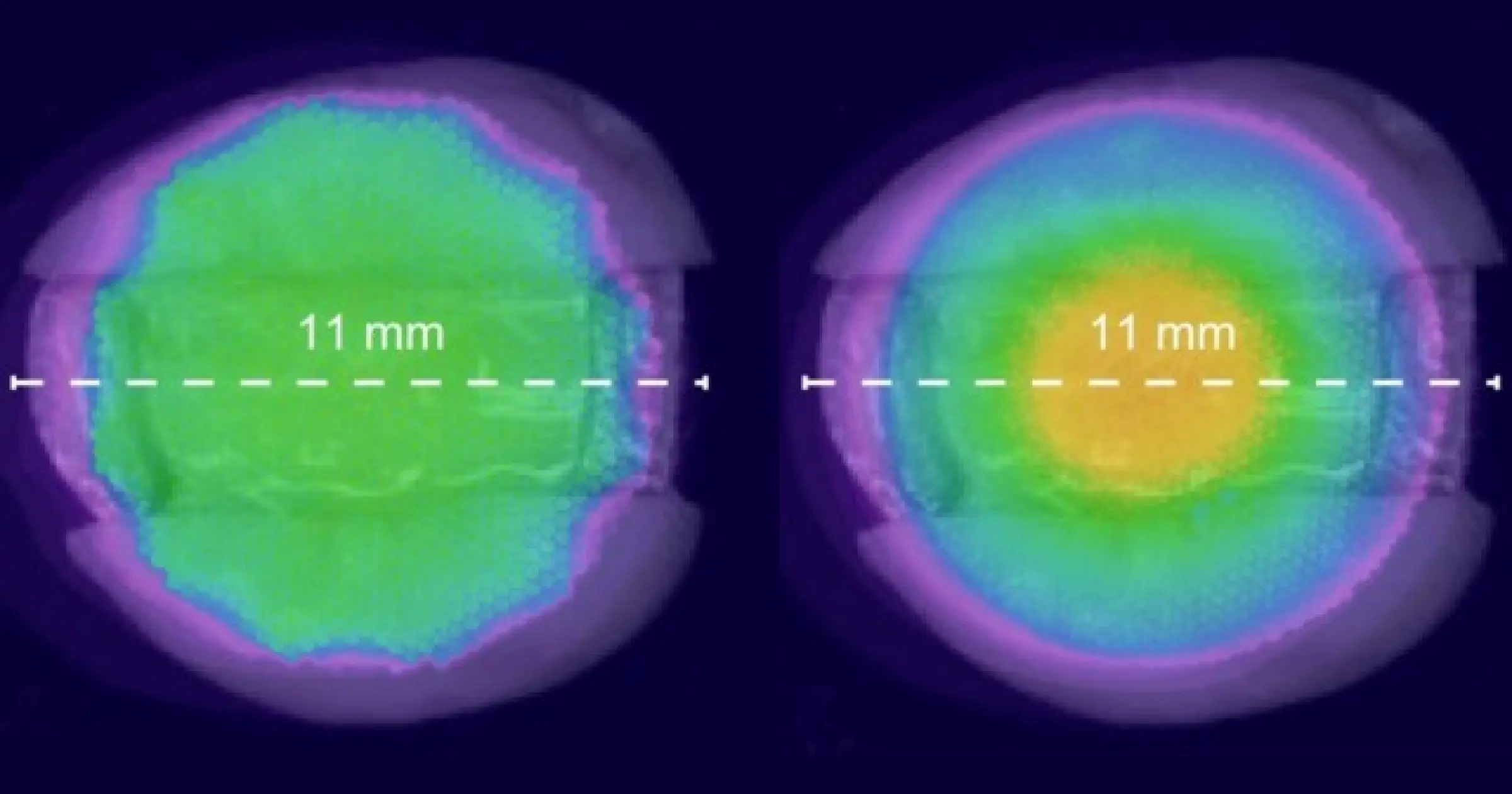
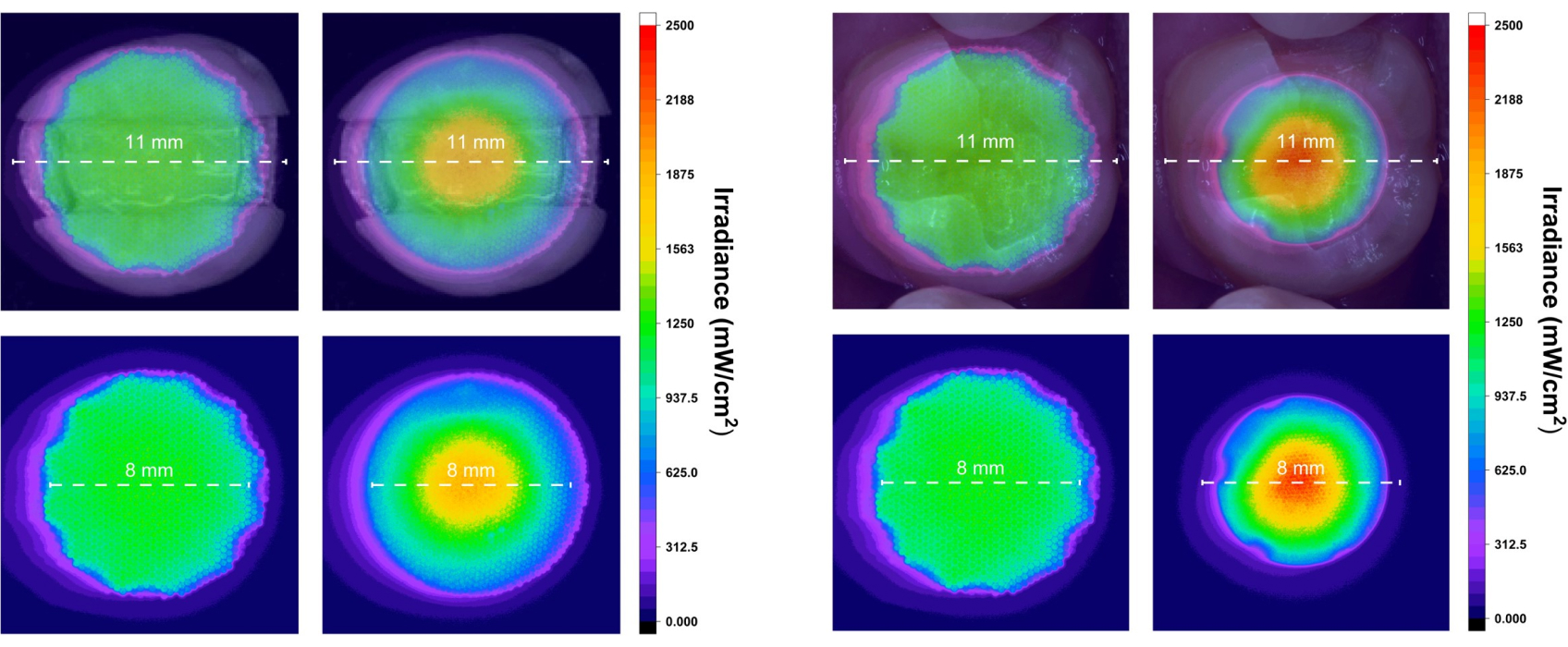
Light beam uniformity is another significant factor in adequate resin polymerization, because the light emitted from curing lights may not be evenly distributed (Figs. 5 and 6).1
There can be “cold spots” or “hot spots” within the light beam, which means certain regions may have adequate light delivery while others won’t attain enough light for complete polymerization.
The varied sizes and circumferences of curing light tips may mean the tip is too small for an extensive preparation, which would result in poor light attenuation and inadequate cure.
Proper positioning and use of the curing light is essential to the resin restorative process. “Light-cure the material” typically is a cue for a chairside assistant, but do your assistants understand the importance and significance of adequate light curing? Without the right training, they may not correctly position and angle the curing light tip or increase the cure time for a particularly deep margin. Curing isn’t as simple as it appears!
“Your wand now contains the power of your enormous courage.”
Light wands and tips that aren’t clean of debris will diminish the irradiance and amount of light reaching the resin materials, so it’s essential to eliminate any accumulated cured resin from the surface of tip ends. Sterilization of curing tips also reduces brightness and luminescence, but covering tip guides with sterilization barriers can significantly reduce light output; some literature shows a 40% reduction in irradiance using protective sleeves. When using a curing device with a removable light guide, cleansing the lens or filter inside the curing light housing should be a routine maintenance procedure.
Clinicians can’t visually evaluate the quality or quantity of light dissipated from the curing light, so there may be a false sense of security about whether the resin is appropriately cured to its complete depth. As curing lights age, their light source degrades and their power decreases. Record the power of the light emissions when the curing light is new and then monitor it regularly with a radiometer for insight into power reductions over time. Radiometers can be expensive, but some manufacturers or sales representatives will provide this service routinely if requested.
“Red sparks flew out of the end.”
It’s well known that cumulative exposure to blue light affects the retina, and the International Commission on Non-Ionizing Radiation Protection has established guidelines about optical radiation. High levels of blue light can cause immediate and irreversible retinal burning, and chronic blue light levels contribute to retinal aging and can accelerate macular degeneration.
The “blue light hazard” is the greatest at 440 nm, the maximum emission from dental light-curing units; a recent study determined that in a normal dental workday, if a clinician not wearing protective lenses looks at the curing light for only the first second, it may take only seven curing cycles to reach the maximum daily recommended dose of radiation. Blue-light-filtering glasses can reduce transmission of light below 500 nm to less than 1%, and wearing orange blocker protection enables clinicians to observe the entire curing process safely.1
“Harry wielded this wand throughout his Hogwarts career and demonstrated his growing magical skill.”
Just like Harry Potter, today’s dentists can perform extraordinary feats of dentistry! Resin adhesives provide tremendous opportunity for natural appearance, longevity, and predictability. This is all the result of managing the polymerization process of resin materials.
Light activation allows clinicians to completely control the setting or curing of restorative material. Understanding the chemical process, function, behavior, and management of light activation provides them the opportunity to work like a wizard with contemporary resin materials.
References:
- Mutluay, MM, Rueggeberg, FA, & Price, RB (2014). Effect of using proper light-curing techniques on energy delivered to a Class 1 restoration. Quintessence International (Berlin, Germany), 45(7), 549–556.
- Rueggeberg, FA, Giannini, M, Arrais, CAG, & Price, RBT (2017). Light curing in dentistry and clinical implications: A literature review. Brazilian Oral Research, 31(Suppl 1), e61.
- Price, RB, Labrie, D, Whalen, JM, & Felix, CM (2011). Effect of distance on irradiance and beam homogeneity from 4 light-emitting diode curing units. Journal (Canadian Dental Association), 77, B9.
SPEAR NAVIGATOR
Transform how your practice runs by engaging the team through
coaching and training
A guided path to excellence through structured coaching and self-guided resources that will align your team, streamline processes and drive growth. Transform your practice by implementing Spear’s proven playbooks for developing and retaining a high-performing dental team.
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.
VIRTUAL SEMINARS
The Campus CE Experience
– Online, Anywhere
Spear Virtual Seminars give you versatility to refine your clinical skills following the same lessons that you would at the Spear Campus in Scottsdale — but from anywhere, as a safe online alternative to large-attendance campus events. Ask an advisor how your practice can take advantage of this new CE option.
FOUNDATIONS MEMBERSHIP
New Dentist?
This Program Is Just for You!
Spear’s Foundations membership is specifically for dentists in their first 0–5 years of practice. For less than you charge for one crown, get a full year of training that applies to your daily work, including guidance from trusted faculty and support from a community of peers — all for only $599 a year.

By: Jeffrey Bonk
Date: April 28, 2025
Featured Digest articles
Insights and advice from Spear Faculty and industry experts