How to Uncover an Implant 101
There are multiple ways to uncover an implant during second-stage surgery. One can either use a tissue punch, a diode laser or a #15 blade; it all depends on whether the practitioner knows the exact placement of the implant and where they want the attached tissue to be.
Every practitioner should have a few of these techniques in their bag of tricks to achieve great tissue esthetics around their final restoration.
If you know exactly where the implant is buccolingually and mesiodistally and there is ample attached tissue, a tissue punch could be the best option. It is a flapless procedure that is extremely time-efficient and allows the placement of a healing collar within minutes.
However, the caveat with this technique is the fact that being off by greater than a millimeter can be quite problematic. You would either have to do a second punch or bring out the scalpel. This can result in exposed bone and secondary healing unless you can manipulate the remaining tissue to cover the exposed bone.
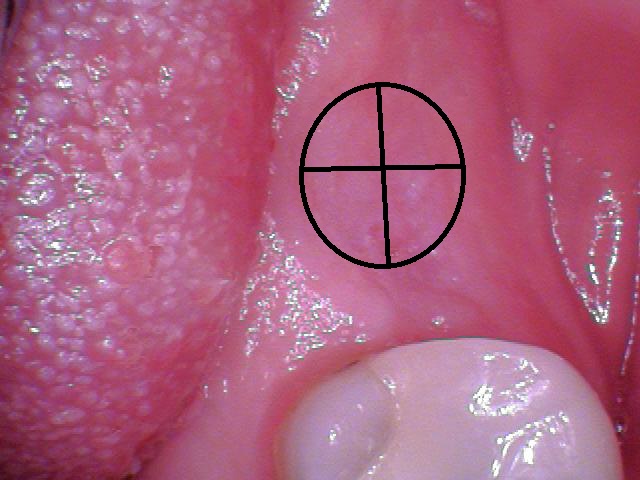
To create the same effect as the tissue punch while promoting faster healing of the tissue, use a diode laser. Start the laser from the center of the cover screw and work your way out to the edges of the implant platform in a circular motion until the implant has been uncovered. This technique is a little more forgiving because if your aim is slightly off but still on the implant, you can self-correct.
Both of these techniques are best used where there is ample attached tissue and implant placement is known.
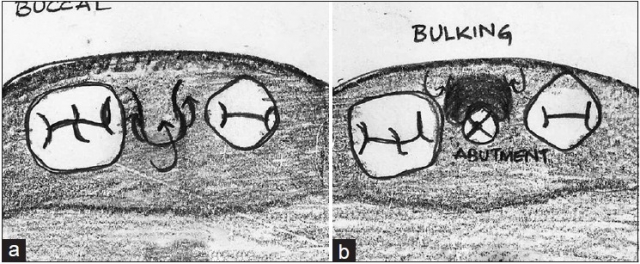
The #15 scalpel can be used in multiple ways and can allow you to place the attached tissue where you want. If you know where the implant is located, you can make two perpendicular incisions over the implant (Fig. 1b). The healing abutment can be placed and the full-thickness flaps can be folded into themselves under the abutment, allowing for ample tissue to surround and heal around the healing abutment.
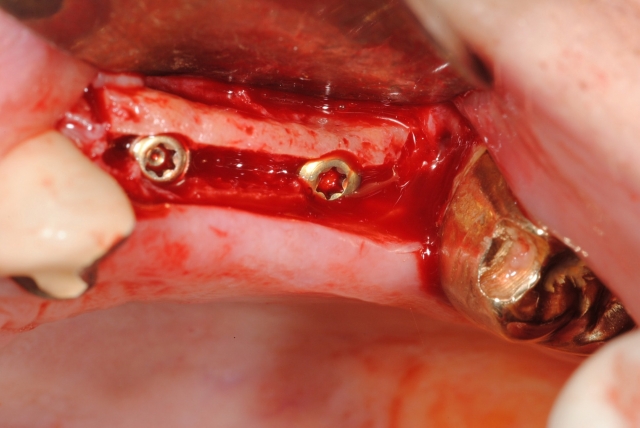
Moreover, if you want greater interproximal attached tissue to increase papillae, turn the cross 45 degrees and make diagonal incisions so that the flaps are mesial and distal (Fig. 1c). The buccal flap can be left as is or removed with a diode laser if there is excessive buccal tissue. If there is ample attached tissue but you are unclear about exact implant placement or have multiple implants to uncover, then you may make a midcrestal incision and expose the implant site(s) (Fig. 2).
These three techniques are best used in the premolar or molar region but can be considered in the esthetic zone if there is ample labial attached gingiva.



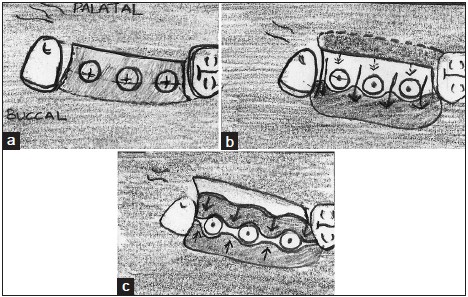
When presented with the predicament of not having enough buccal attached tissue to gain the esthetic outcome desired on the final restoration, the following technique allows one to move all the attached tissue covering the implant site over to the buccal.
Start by making a U-shaped incision that goes well around the implant site (Fig. 3a). Release the flap, deepithelize it, then roll the flap and tuck it underneath the buccal pouch (Fig. 3b). This will bulk the attached tissue on the buccal.
Another way, as seen in Figs. 4a–4c, is to start by placing a midcrestal incision aimed lingual to the implant site, then following the lingual border of the implant platform and finishing the midcrestal incision. Release the full-thickness flap and bring all that attached tissue over to the buccal. Then a pediculated full-thickness palatal flap would be rotated to closely adapt to the healing abutments. This allows for preservation of all the attached tissue and effectively increases the buccal attached tissue significantly. This technique is best for any area that does not have enough buccal attached tissue or to increase buccal attached tissue, especially in the esthetic zone.
Reference
- Phadke P, Rajeshwari H, Sapna N, Suchetha A. Optimising esthetics in second stage dental implant surgery: Periodontist’s ingenuity. Journal of Dental Implant. 2014; 4(2):170.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Puneet Sandhu
Date: December 22, 2017
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


