The Guide to When and When Not to Splint Restorations
There are a lot of clinical situations that arise that beg this question: Should the teeth or restorations be splinted or not?
I’m not referring to cases in which there are missing teeth — of course, these situations require splinting. I am referring to situations where all the teeth are present. Although not all situations can be addressed in one article, the following should help answer a few questions.
These are general guidelines and are not applicable to all clinical situations. The question, once again, is whether the teeth or restorations should be splinted.
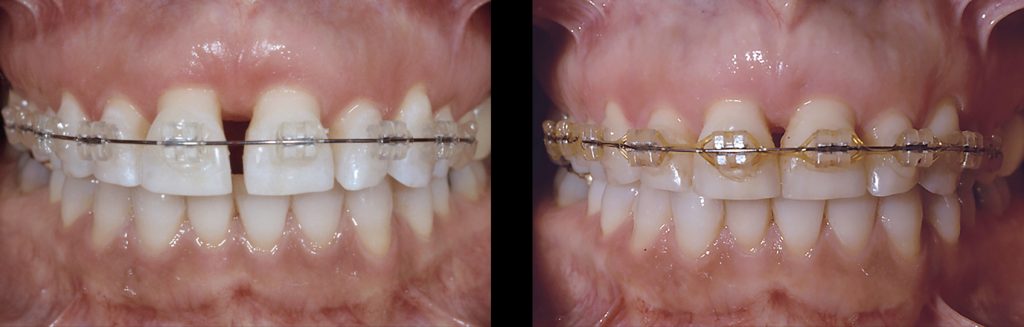
Provisionals: Yes
Splinting provisionals offers numerous benefits. It enhances the strength and retention of the provisionals, making fabrication easier. The only time I wouldn’t splint provisionals is before orthodontics, where the teeth need to be able to move independently. When restoring an arch of teeth, it is typically easier to keep the provisionals in three segments (an anterior segment — cuspid-to-cuspid — and two posterior segments).
Patient with bruxism or grinding: No
It has been stated that splinting restorations in these types of situations makes the teeth stronger and more able to withstand the force. The reality is that when teeth are splinted together, the entire system becomes more rigid. If a patient has significant signs of attrition, I want the teeth to be able to move individually in response to the force. This “shock absorption” helps to prevent fractured ceramic.
In addition, if there is a failure of an individual restoration, the more teeth that are splinted together, the more difficult and costly the repair will be. If the restorations are kept as individual units, the repair or replacement is much easier.
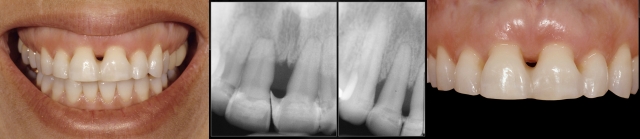
Mobile teeth: Yes
Splinting teeth with mobility due to short roots resulting from a history of periodontal disease, short roots caused by root resorption, or excessively tapered roots can be beneficial. This is especially true if they can be splinted to a tooth (teeth) that is not mobile, as it will help create stability. Even splinting multiple mobile teeth together can help create stability, especially if the teeth that are splinted turn the corner of the arch. The reason splinting can be helpful is that all teeth are mobile in the same direction (buccal-lingual); however, depending on where the teeth are positioned in the arch, their buccal-lingual direction may vary in different vectors.

Structurally compromised teeth: Yes
Splinting teeth that are structurally compromised (i.e., lacking adequate tooth structure or short preps) is similar to double abutting multiple-unit FPD restorations for added structural stability. Although it must be said that if the tooth is that structurally compromised, it might be advantageous to consider removal of said tooth and replacement with an implant.
Implants: Depends
Implants already create a rigid system, making the restorations more prone to ceramic fracture. Therefore, the main reason to splint them would be to distribute stress (from horizontal forces) and minimize excessive load on individual implants or components. My rule of splinting implants depends on multiple factors.
1. External hex (Branemark-style) implants: Yes
The external hex on these implants provide little resistance or retention to the abutments, so a lot of load is placed on the screw itself. In these situations, splinting the implant restorations can be advantageous. However, due to the rigidness of the system and the tolerance in the fit of the components, trying to create well-fitting restorations with passive fit in these types of situations can be challenging.
2. Internal connection (platform switch) implants: No
Today’s implants are primarily designed with an internal connection that utilizes a platform-switch concept. With this design, the screw gets minimal load, as most of the forces are distributed in the internal connection. In these situations, splinting the restorations is typically not as advantageous. If the restorations are treated as single units and an individual restoration has a problem, repair and/or replacement of the restoration is much easier and less costly.
3. Short implants: Yes
There are times when the length of the implant that can be placed is limited due to the local anatomy. In these situations, it may be beneficial to splint the implant restorations together to help biomechanically (Yang TC., Int J Prosthodont, 2011). However, it must be noted that if the length of the implant crown is 15 mm or greater, splinting the implants together did not help prevent prosthetic failure regardless of the implant length (Nissan J., J Oral Maxillofac Surg, 2011).
4. Implants and natural teeth: No
The literature is clear that it is not a good idea to splint implants and natural teeth (Rangert B., Int J Oral Maxillofac Impl, 1991). When an implant and a natural tooth are connected, the forces applied to one now affect the other. The amount of force transferred varies depending on the amount of mobility of the natural tooth. Connecting teeth and implants never increases the load on the tooth … only on the implant.
The only time implants and natural teeth can be connected without risk is in situations where the natural teeth provide no support for the FPD. In other words, ask yourself: “Would the restoration still be structurally supported if the teeth were pontics?” If the answer is yes, then the implants and natural teeth can be splinted.
For example, can you splint implants in #7 and #10 to central incisors with a Grade II mobility? Imagine if the central incisors were pontics. Would an implant restoration from #7-10 be structurally sound? YES! In this situation, the natural teeth provide no structural support for the restoration, but they do help maintain the soft tissue architecture and overall esthetics.

FOUNDATIONS MEMBERSHIP
New Dentist?
This Program Is Just for You!
Spear’s Foundations membership is specifically for dentists in their first 0–5 years of practice. For less than you charge for one crown, get a full year of training that applies to your daily work, including guidance from trusted faculty and support from a community of peers — all for only $599 a year.

By: Greggory Kinzer
Date: January 22, 2018
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


