The Role the First Point of Contact Plays in the Restorative Process
Identifying the first point of contact when conducting patient examinations increases the effectiveness of restorations when planning treatment.
Patients have the ability to adapt to a wide variety of occlusal contact positions — from complete unawareness on one end of the spectrum, to a tolerance of less than the thickness of Shimstock on the other end. Identifying the first point of contact provides an opportunity to have a discussion with the patient, build trust, and draw them into the decisions that are involved in restorative treatment.
Spear articles and courses demonstrate the use of the leaf gauge and the Lucia jig. Working with these two instruments aims to find the fully seated condylar position (FSCP): the position where the lateral pterygoids relax and serve as a starting point for mandibular movement.
The ‘Why’ Behind Finding the First Point of Contact
Identifying the FSCP is where the first point of contact between the upper and lower teeth becomes visible. This article focuses on two contrasting scenarios to emphasize the “why” behind finding the first point of contact.
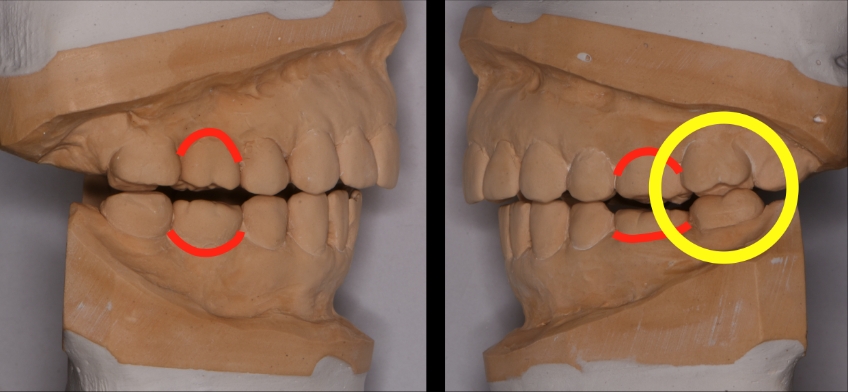
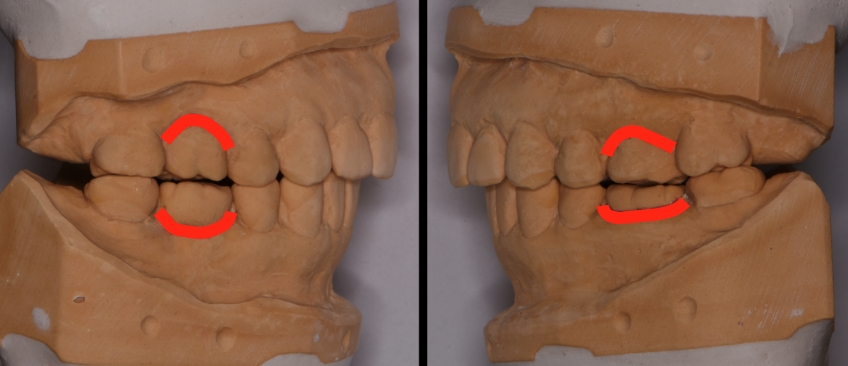
The first set of models shown here is for a patient for whom we have decided to remake the first molar crowns. The first point of contact was identified in the FSCP between teeth #15 and #18 (2-7 & 3-7). The patient explained that she has had sensitivity with #18 for many years, has had root canal treatment, and has had the tooth re-evaluated by the endodontist as it continues to be sensitive. Then the patient asked, “Should we just remake this crown while working on the other teeth”?
The information obtained from identifying the first point of contact begins to find answers to specific questions. For instance, would an occlusal adjustment create a favorable modification to the existing contours and occlusal contacts? How would the patient respond to the modifications? Would the changes be within the patient’s range of adaptability? An occlusal modification can be additive, subtractive, or a combination. Is there a way to recover from the modifications made? Are the existing occlusal contacts a result of an altered TMJ complex on one side? Is there a history of trauma?
At this point, with more information available, it’s possible to present options to the patient. Load testing using a leaf gauge or Lucia jig would be used to evaluate the position of the medial pole of the disc. With no pain or discomfort from load testing (and no reported pain or discomfort related to the TMJ complex), it may be logical to move forward with restorative treatment. Imaging of the TMJ is a way to evaluate the current anatomy and to serve as a reference point in the event of future changes.
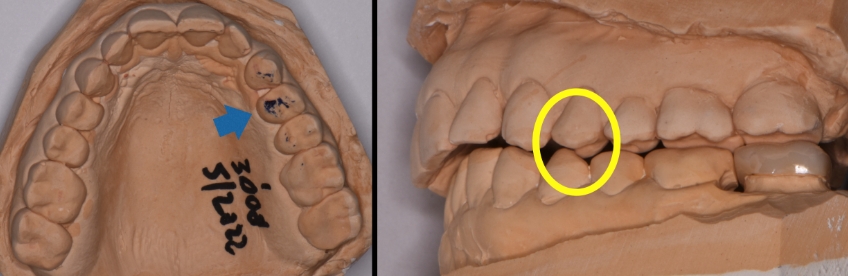
The outcome of the occlusal adjustment is contact in the posterior premolar and second molar areas. The opportunity is to evaluate how the lower second molar responds to the modifications. Will it remain sensitive (potential for fracture or a challenging endodontic re-treatment scenario) or improve? This tooth can be treated as a single area of focus instead of creating the potential that #18 might lead to the restorative treatment in the patient’s mind.
The opportunity also exists to evaluate further: a maxillary occlusal appliance may prove helpful. At this point, when the lower restorations are made, the appliance can be modified/adjusted, as opposed to making a new splint or orthotic.
Let’s take a moment here to think about patient reactions. How would you work with a patient who has not consented to the occlusal adjustment? For example, what would you do when the first point of contact is identified, the models are mounted, and the patient decides not to proceed with an occlusal adjustment? For whatever reason, the patient’s mindset is focused on the idea that they have come in for dental work on one tooth, a full-coverage restoration for the lower left second molar. The patient might also think that whatever you do is irrelevant to them. These are all concerns and objections that you need to be ready for.
So, getting back to our clinical analysis, the first contact in the fully seated condylar position (FSCP) was identified to occur between inclined surfaces at the left side first premolar. It would be reasonable for the positioning muscles to alter the mandible forward of the FSCP to avoid a deflective contact. A pattern of muscle memory would develop where the patient would not be consciously aware of the protective mechanism in place to avoid a deflective contact.
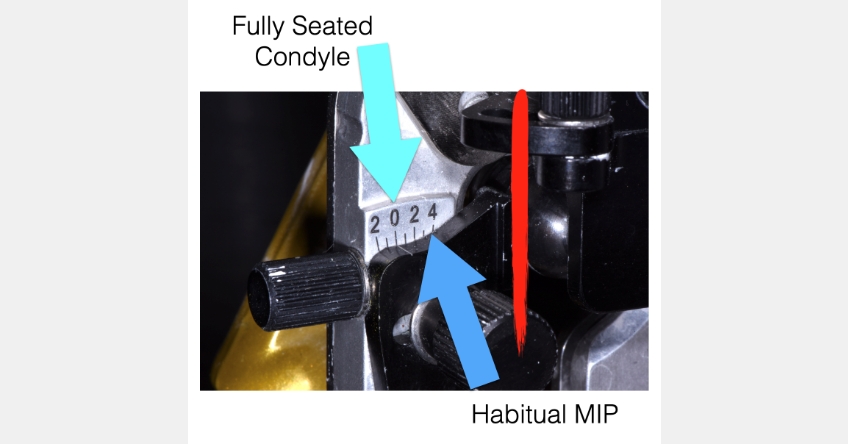
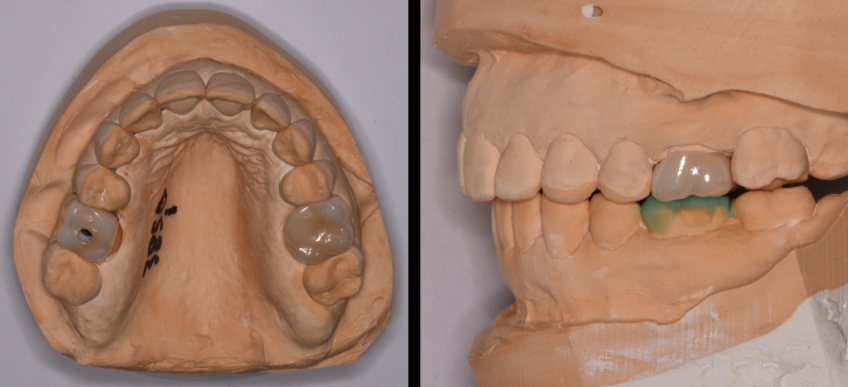
This is where having a full set of models mounted on an adjustable articulator provides information helpful in the outcome of the definitive restoration. At this point, I can set the condylar element on the articulator to mimic the centric occlusion where the mandible is positioned forward of the FSCP. The full coverage restoration for the lower left second molar can be made matching the wear facets of the natural tooth surfaces, as well as the contours of the existing restorations.
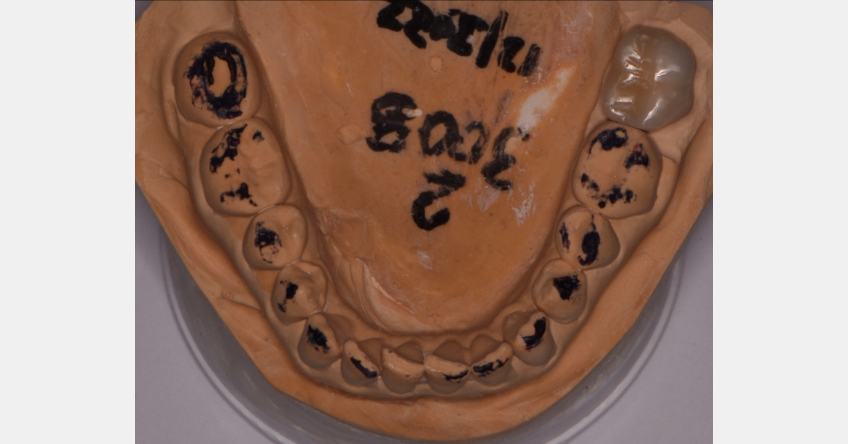
The time spent refining the restoration on the models reduces the clinical chair time required for insertion. The process helps to identify potential areas of concern when leaving the first point of contact as identified. Once the refinement of the restoration has been completed, the models can be modified to simulate an occlusal adjustment/equilibration and note the impact on the second molar only to see what might happen. This is an opportunity to draw the patient into the process and provide a couple of things to look for as a warning signs, further demonstrating your focus on their dental care.
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Doug Benting
Date: April 6, 2023
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


