A Business Model for TMD and Airway Dentistry
Since 3D imaging assesses patients’ anatomy more accurately than ever before, more patients than previously assumed are being discovered with compromised temporomandibular joints (TMJ) and the airway system. While 3D imaging is vital to understanding many presenting problems, dentists are often challenged when it comes to developing a practice model that allows for a reasonable fee to maintain practice profitability.
Traditional dental practice generates revenues from restorative procedures necessitated by tooth loss due to decay. Yet, the profession’s knowledge base has grown, and the amount of decay in patients has decreased.
These days, it’s relatively routine for dentists to see patients with little to no decay who only need minimal restorative dentistry. However, many patients do have serious issues beyond restorative ones. Patients with significant alterations in normal joint anatomy, because of poor mandibular and maxillary growth, have decreased oropharyngeal airway anatomy.
Compromised Oropharyngeal Airway Space
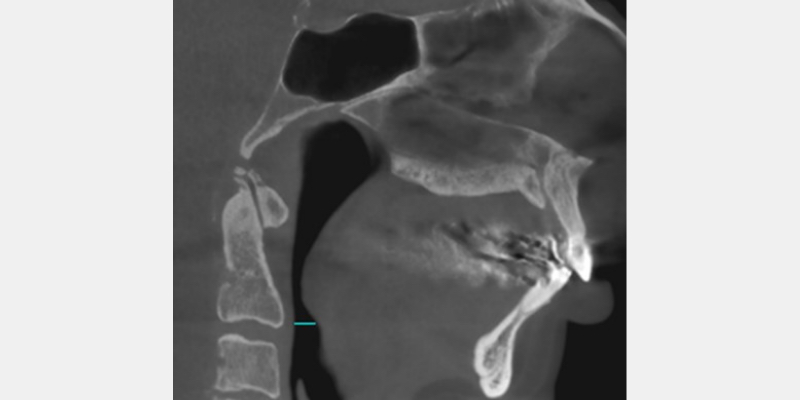
George, a 57-year-old male (Fig. 1), has small condyles, which usually correlate to an injury to the TMJ occurring before growth is complete. In a 2006 journal article, Carlos Flores-Mir and Brian Nebbe1 discuss an atypical TMJ disc abnormality associated with reduced forward growth of the maxillary and mandibular bodies.
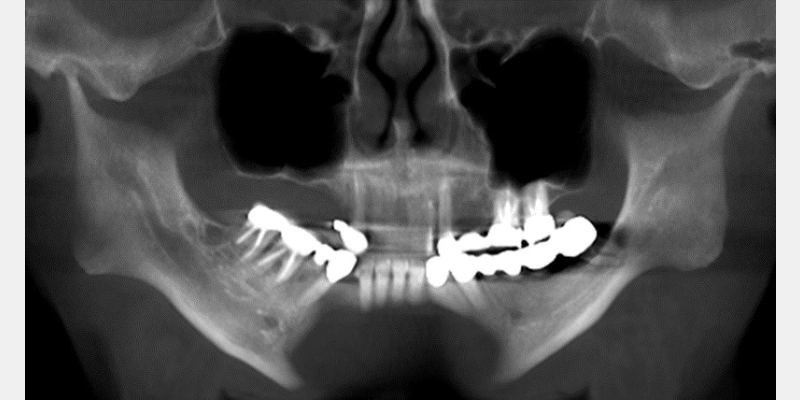
In many cases, they studied, reduced maxillary and mandibular growth resulted in a compromised oropharyngeal airway space. (Fig. 2)
To help a patient like George, a practice must create a diagnostic system that allows the practitioner time to evaluate the TMJ and the airway. This requires additional diagnostic information, different from that obtained in a traditional restorative practice model. Traditionally, restorative patients require mounted study casts with photographs to develop a treatment plan.
More information is needed to develop a treatment plan for patients with TMD and airway issues. In most cases, an MRI, a CBCT, and a sleep screening may be necessary to understand the appropriate treatment options.
When treating these patients, significant time is required to post-process and study the imaging and sleep screening. To obtain this information and have a sufficient period to study it, it’s necessary to create a multi-appointment process so there is enough time to plan the treatment of these cases.
The first appointment in this process is a typical new patient examination, designed to gather data and determine if additional diagnostic information (e.g., MRI, CBCT, sleep screening) is needed. If the findings in the history and clinical exam warrant additional diagnostic information, the case presentation for the diagnostic records and consultation occurs at the end of the new patient exam.
Diagnostic Imaging Acceptance
To increase the likelihood of case acceptance for diagnostic records, it’s vital to take an organized approach to educating the patient about normal anatomy and how items reported in the history or noted in the clinical exam typically correlate to structurally altered anatomy.
If a patient presents with a facial asymmetry, it’s easy to explain that normal anatomy leads to normal ramus length and facial anatomy. An injury to TMJ in the growing years can result in a decreased ramus length, resulting in a facial asymmetry and, in some cases, a compressed oropharyngeal airway space. The patient must understand that diagnostic records are the best way for the dentist to make appropriate treatment choices for their case.
In addition to the clinical aspect of creating value for diagnostic records, the financial aspects of obtaining them must be discussed. The patient must understand that many, if not most, insurance companies limit coverage for diagnostic records.
The patient must also understand that reliable treatment recommendations cannot be made without the benefit of the information gained through the judicial use of diagnostic records. Patients who understand their clinical needs and the uncertainty of insurance reimbursement can make decisions based on realistic information.
Fees for Diagnostic Workups
The fee should be determined by the number of hours of the exam and diagnostic records appointments. The combined time for the exam and records appointments can be multiplied by the hourly rate necessary to run the practice, and a fee can be set for the exam and the diagnostic records.
Over the years, I’ve allocated this fee between the exam and the diagnostic records. When discussing with potential new patients over the phone, I set a lower exam fee to remove the barrier of high fees. I make up the difference from the decreased exam fee in the diagnostic records fee once I’ve had the opportunity to meet the patient and create value for diagnostic records.
The consultation fee is included in the diagnostic records fee. The consultation typically lasts between 30 and 60 minutes and offers the opportunity to review normal anatomy, explain structurally altered anatomy, discuss treatment options, and choose the most appropriate treatment. Once the most appropriate treatment options are discussed, the fee and any insurance information can also be reviewed with the patient.
In my experience, the model of a lower exam fee and a higher diagnostic records fee leads to a predictable pathway for patients to benefit from a comprehensive treatment plan when necessary. This business model works well for both TMD and airway patients, allowing a fair fee for the diagnostic workups necessary in these cases.
References
- Flores-Mir, C., Nebbe, B., Heo, G., & Major, P. W. (2006). Longitudinal study of temporomandibular joint disc status and craniofacial growth. American Journal of Orthodontics and Dentofacial Orthopedics, 130(3), 324-330.
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Jim McKee
Date: July 10, 2020
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


