Autogenous Fat: Preferred Material for TMJ Disk Replacement
Most people reduce their abdominal fat to look and feel better. Still, some temporomandibular joint (TMJ) patients use abdominal fat to help treat the TMJ problems that have plagued them for decades.
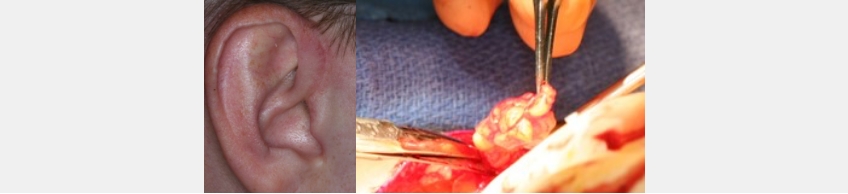
In normal jaw joints, ligaments attach a disk to the lateral and medial poles of the condyle, but if the ligaments tear, a diskal herniation can occur. Treatment for TMJ patients presenting with ligament tears and either large 11:00 discs, eroded condylar bone, small condylar bone, or edematous condylar bone means changing TMJ’s soft- or hard-tissue anatomy.
While disc repairs are the preferred option to restore normal joint anatomy, they are not possible in many patients, given the amount of soft- or hard-tissue deformation. In these cases, replacing the disc with abdominal fat may be possible.
The Fat Advantage
Sachin Rai discussed this option in his 2021 article, “Autogenous Fat as an Ideal Interpositional Material in Temporomandibular Joint Surgery.” Rai outlines the procedure, which started in the latter half of the 1800s. While other materials have been used to replace the disk, fat has the advantages of being readily abundant, easy to harvest, minimally morbid, and having long-term survival.
From a biologic perspective, fat offers the advantages of encouraging hemostasis and inhibiting osteogenesis, which reduces the chance for joint ankylosis. Fat grafts undergo a period of initial breakdown of fat cells, followed by revascularization, resulting in normal-appearing fat, although in a smaller volume than originally grafted.
Fat volume usually decreases by 33-50% during the first year of healing, and while patients may be concerned with visible scarring, this is rarely a concern with careful surgical techniques.
From an occlusal perspective, replacing the disc with fat increases the vertical dimension at the TMJ level and typically results in a posterior open bite. It is critical to the success of the disc replacement to support the post-surgical joint vertical dimension, using several possible clinical procedures.
The usual protocol has been to use a stabilization appliance that allows the fat to vascularize over 6-9 months. The appliance limits the ability of the condyle to move superiorly and compresses the fat before revascularization occurs. After the initial 6-9 months of healing, the posterior open bite can be addressed through orthodontics, direct restorations with composite, indirect restoration with different materials, or a combination of these options.
Once the fat revascularizes and the occlusion stabilizes, many patients experience dramatic decreases in pain and increases in quality of life.
Reference
- Rai, S. (2021). Autogenous Fat as an Ideal Interpositional Material in Temporomandibular Joint Surgery. Journal of Maxillofacial and Oral Surgery, 20(4), 527-533.
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Jim McKee
Date: April 4, 2022
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


