OSHA and CDC Guidelines for Dentistry: Training Your Dental Staff on Bloodborne Pathogens
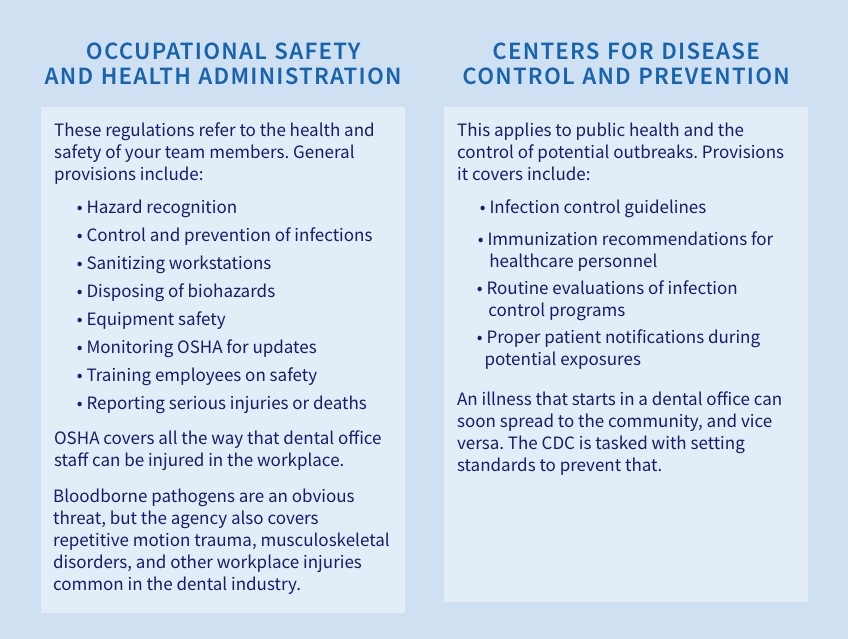
There is much overlap between the Occupational Safety and Health Administration (OSHA) and the Center for Disease Control (CDC) guidelines for dentistry. While both government agencies are designed to protect the public’s health, they do it in different ways. OSHA controls what happens inside the dental office, while the CDC focuses on preventing outbreaks that can start in dental offices, where bloodborne pathogens are an ever-present threat. Following both OSHA and CDC guidelines in dentistry helps control these risks.
General OSHA and CDC guidelines for dentistry
The easiest way to remember the difference between OSHA and CDC guidelines for dentistry is to remember that one pertains to the health of team members, and the other applies to the health of the public.
In a dental office, OSHA and CDC guidelines meet regarding bloodborne pathogen training. The control of the spread of infectious diseases like HIV, as well as Hepatitis B and C, are primary concerns, but there is a wide-range of risks team members face outside of these conditions.
Effectively managing bloodborne pathogens in dental offices
“Bloodborne pathogens” is commonly used to refer to training on HIV and hepatitis infection controls, but the category has grown in the face of COVID-19 and new threats. The CDC sets its guidelines around prevention, training, and responding to incidents.
When it comes to specific bloodborne pathogen requirements, the CDC follows OSHA guidelines, which simplifies things. Here are broad categories around bloodborne pathogens you can review:
Immunizations
The CDC recommends health care professionals, including dental team members, be immunized against Hepatitis B, influenza, measles, mumps, rubella, pertussis, and varicella. For COVID-19 vaccine requirements, it refers providers to their specific state dental board for guidance.
It also suggests that individuals with certain health conditions, or those who work outside the U.S., consider vaccinating against meningococcal disease, typhoid fever, and polio. Tuberculosis screening for all team members before they start is also required.
Education and training
Any employee exposed to blood or other infectious biological material must have annual bloodborne pathogen training. This training is required regardless of any previous education or training, and there is no exemption. It must also be conducted if you change procedures in a way that could put team members at a new exposure risk.
OSHA mandates the following areas be covered regarding this training:
- Information on bloodborne pathogens and diseases
- Methods used to control occupational exposure
- Information and access to Hepatitis B vaccines
- Medical evaluation and post-exposure follow-up procedures.
Finally, the training needs to be presented in a way that is appropriate for the team’s educational level and language. Many dental practices fall flat here, because they use a single training program for all staff when it’s not necessarily appropriate. Make sure your training is presented in a position-specific way that is targeted to the individual team members to avoid this.
Needlestick prevention
The CDC estimates there are about 385,000 needlestick injuries per year in the U.S. — and it admits estimates are off, because these may be underreported in some settings. Employees in a dental office are at particularly considerable risk because they use needles in a very enclosed space, putting them at a greater chance of exposure. A proper needlestick program ensures individuals know how to safely handle sharps, how to dispose of them, and what to do if they are injured by a contaminated instrument.
Infection program evaluation
A good infection program has clearly developed operating procedures and practices. It has processes to document any adverse incidents, like blood exposures or infections. This also applies to OSHA reporting standards for needlesticks and sharp injuries.
The employer must maintain a clear log that covers the type and brand of device that caused the injury, the area where the incident took place, and an explanation of how the injury happened. Remember that this information is also private medical information for the employee; if it is shared with an outside party, all identifying information on the employee should be withheld.
Most of the topics on OSHA and CDC guidelines in dentistry are focused on bloodborne pathogens. With a detailed program in place and strong reporting methods, you can maintain safety in the workplace and limit the spread of infectious, dangerous diseases.
SPEAR NAVIGATOR
Transform how your practice runs by engaging the team through
coaching and training
A guided path to excellence through structured coaching and self-guided resources that will align your team, streamline processes and drive growth. Transform your practice by implementing Spear’s proven playbooks for developing and retaining a high-performing dental team.

By: Spear Team
Date: January 17, 2023
Featured Digest articles
Insights and advice from Spear Faculty and industry experts