Implant-Supported Fixed Bridge for Maxillary Incisors
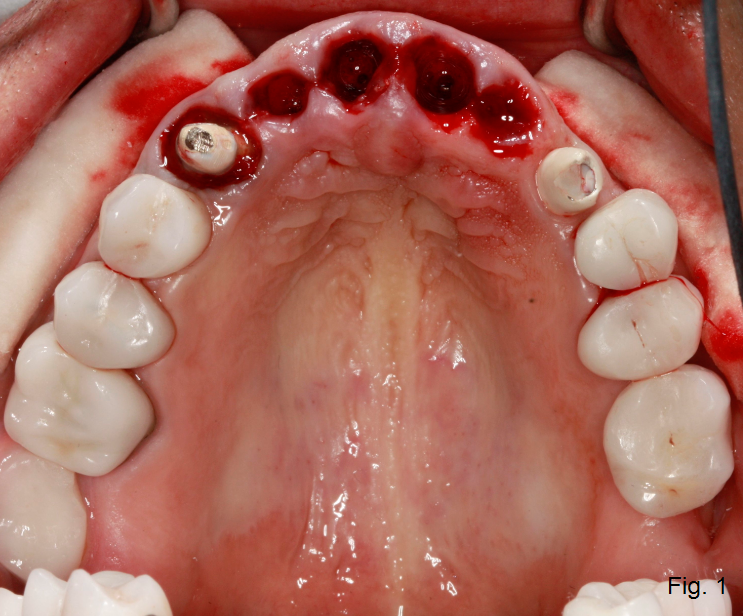
This patient has decided to have his upper maxillary incisors removed following a significant dental history that includes endodontic treatment, clinical crown lengthening, full coverage restorations, and trauma. (Fig. 1)
Indeed, several restorative options are available for treatment: tooth-supported fixed bridge, dental implant-supported fixed bridge, individual dental implant-supported restorations, removable partial denture, and, of course, no treatment. When there are several options available, it’s our responsibility to help the patient decide on the options available based on their unique situation and circumstances. For the sake of discussion, let’s assume that the patient is interested in a dental implant-supported fixed bridge restoration in the anterior maxillary segment. What would you like to know based on what you see in the clinical photo?
A Couple of Thoughts before we Discuss the Implant-Supported Fixed Bridge Option
Fresh extraction sites visible in the photos certainly lead us to consider whether the labial plate of bone is intact or fractured for each of the incisors. Will augmentation or grafting be indicated? If so, how will that impact the provisional restoration? What about lip length and lip mobility — particularly regarding gingival display? What characteristics are you looking for in an implant system that could help with the restorative treatment goals?
Back to the dental implant-supported fixed bridge — there are several options available. Two dental implants could be placed in each of the lateral incisor positions (#7 and #10), or the central incisor positions (#8 and #9), or an alternating scenario that includes a lateral incisor position and a central incisor position (#7 and #9, for example).
In an article by Correa1, the effect of implant position on the displacement of the prosthetic structure and the displacement of the supporting bone was studied at forces applicable to the anterior maxilla. The implant-supported fixed bridge was the least displaced with the implants in the central incisor positions, although the flexure was shown to be concentrated in the supporting alveolar structures.
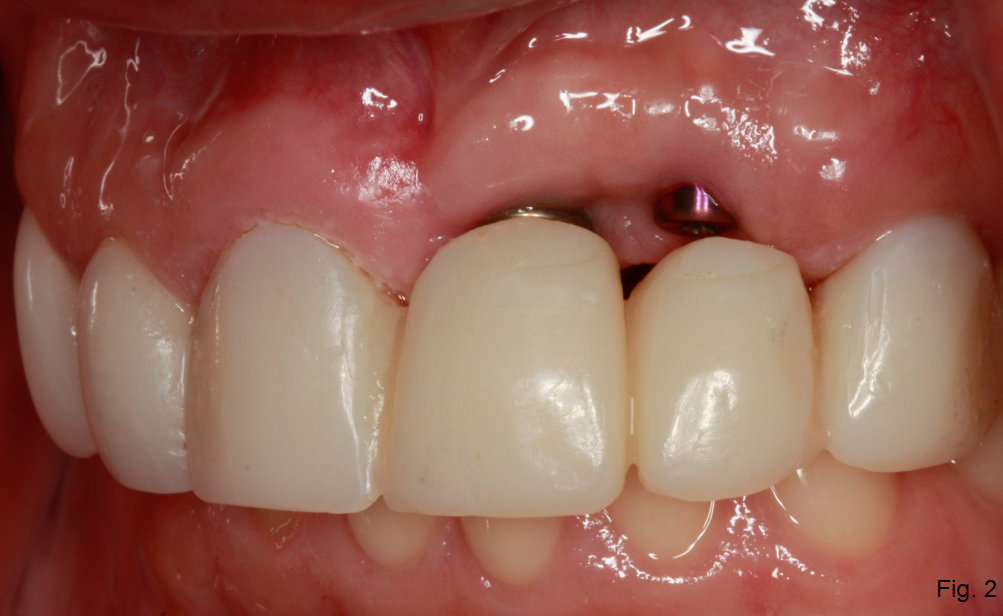
We often think about tissue thickness in a pontic site versus an area with a dental implant-supported restoration. Other times, a concern arises as to the labio-lingual thickness of bone in the lateral incisor positions or, with the “wagon wheel” effect, if the implants can be placed close enough to the canines to truly be in the lateral incisor position instead of the interproximal space between the laterals and the centrals. (Fig. 2) In other scenarios, dental implants in the central incisor position could be palatally oriented to a point that could affect cervical contours and speech sounds. Regarding restorative flexibility, where would you like the implants placed to facilitate the option for natural gingival tissue or prosthetic pink ‘tissue’?
Reference
- Corrêa, C. B., Margonar, R., Noritomi, P. Y., & Vaz, L. G. (2014). Mechanical behavior of dental implants in different positions in the rehabilitation of the anterior maxilla. The Journal of Prosthetic Dentistry, 111(4), 301-309.
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!

By: Doug Benting
Date: January 21, 2019
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


