Simple In-Office Technique for Closing Open Molar Contacts
Proximal contact areas maintain the integrity of dental arches. The anterior force of occlusion has been shown to stabilize the dental arches and help maintain proximal integrity. Teeth are stabilized by contact with adjacent teeth and occlusal contact with the opposing tooth. Weak or slightly open contacts can create issues for patients regarding chewing comfort and maintenance. Open contacts may allow for food impaction, which can be very discomforting to patients.
Long-standing open contacts could create periodontal inflammation and subsequent bone loss, which can contribute to more extensive tooth migration and occlusal disharmony. Additionally, dental caries is another concern related to food impaction. Therefore, maintaining proper proximal contact in natural dentitions is essential.
Proximal Contact Strength
Proximal contact strength (PCS) is generally measured by passing floss through the interproximal surfaces of the teeth. The presence of a “snap” signifies that adequate tooth contact exists. This determination is unscientific.
Numerous articles in the literature measure proximal contact strength (PCS). PCS is not a constant value. Various teeth and dental arches have differing measurements. The magnitude is the critical aspect that affects clinical situations.
C.E. Dörfer and a team studied PCS and concluded in the European Journal of Oral Sciences that proximal contact force is a physiological entity of multifactorial origin. They determined that PCS is lower in the maxilla than in the mandible.
In the study, the lowest contact strength existed between the upper canine and the first premolar, and the highest between the lower premolar and the first molar. Not only was it determined that contact tightness varied between tooth location and the time of day (morning vs. afternoon), but chewing and mastication also contributed. Body posture and positioning have also been shown to be contributing factors to contact tightness and change.
Clenching forces, such as teeth being displaced, have been shown to contribute to the opening of contacts. Open tooth contacts can be frustrating for both patients and dentists, as food impaction can cause gingival inflammation and bleeding. Managing these open contact situations is vital to maintaining periodontal health and restoring the stability of occlusion.
Restoring open proximal contact is a viable option for managing these situations; however, restoration alternatives are significant in cases where virgin teeth exhibit open contacts. Here is a simple technique that can easily and effectively manage open contacts in the molar region.
Fabricate in the Dental Office

I will use a clinical example to describe and outline the technique for closing interproximal spaces. My patient, Matt, scheduled an appointment to evaluate an open proximal contact of his second maxillary molar. (Fig. 1)
He complained of food trapping, gingival irritation, and bleeding. Matt has a history of clenching but does not wear a protective occlusal splint. At age 40, he has had no dental restorations and is caries-free. As a regular flosser and a consistent dental re-care patient, this situation was frustrating and irritating to him. He asked for a solution to this concerning problem.

The technique applied to these situations is very simple and easily managed in the dental office (versus dental laboratory collaboration). Once the open contact has been verified, an evaluation and correction of occlusal contact is performed (Fig. 2). Opposing “distal wedging” forces are adjusted and corrected. Elimination of these occlusal contacts is paramount for successful proximal contact management and closure. An alginate impression is obtained and poured in hard stone (die stone).
The contact closure technique can be applied once the poured model is hardened and trimmed. Horizontal parallel lines are scribed on the buccal (and lingual, if desired) aspect of the stone teeth involved in the open contact. Extend the lines at least one tooth forward of the open contact. These lines are used as re-positioning reference points once the die cuts are completed.

Separate the distal tooth from the stone model using a plaster saw or a rotary disc. Separate the tooth directly at the stone model’s mesial and distal contact points (Fig. 3). Once the vertical cuts are complete, detach the tooth by making a horizontal cut approximately 2-3 mm gingival to the facial/buccal gingival margin. I utilize a plaster saw for the vertical cuts, followed by a lab engine and a #557 straight shank cutting tool for the horizontal sectioning.
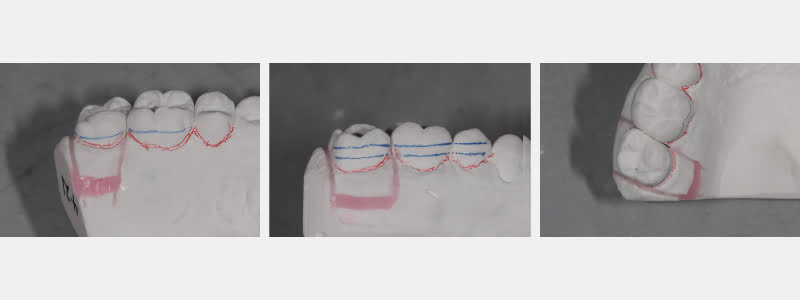
The separated tooth is then reset in the stone cast with wax (Fig. 4). If needed, the proximal contact of the freed tooth is contoured to allow for increased tightness and sufficient contact closure. This tooth is secured with pink baseplate wax. The scribed lines allow for proper positioning in a vertical dimension.

An aligner tray is fabricated on the corrected cast with the contact closed and the stone tooth secured. The Great Lakes MiniSTAR vacuum system is efficient in fabricating well-fitting aligner trays (Fig. 5). Clear Splint Biocryl 1.0 mm tray material is the recommended thickness for efficiently moving the tooth and closing the contact. The aligner tray is trimmed to the buccal and lingual gingival margins.
The patient is instructed to wear the aligner for approximately 20 hours per day. The tray should only be removed for eating and home care maintenance. In my experience, most contacts are fully closed within 2–3 weeks. At that point, the patient is “weaned” from all-day aligner wear to nighttime only. If appropriate, a bruxism/occlusal splint may be fabricated to replace the aligner tray as a long-term occlusal management solution.
This simple tray closure technique has been a game-changer for circumstances in which open posterior contacts have occurred. These aligners are not only well accepted by patients but also create an opportunity to manage frustrating circumstances in a practical and noninvasive manner. I hope this simple technique is as effective and efficient as mine.
References
- Kim, H. S., Na, H. J., Kim, H. J., Kang, D. W., & Oh, S. H. (2009). Evaluation of proximal contact strength by postural changes. The Journal of Advanced Prosthodontics, 1(3), 118.
- Kasahara, K., Miura, H., Kuriyama, M., Kato, H., & Hasegawa, S. (2000). Observations of interproximal contact relations during clenching. International Journal of Prosthodontics, 13(4).
- Oh, S. H., Nakano, M., Bando, E., Shigemoto, S., & Kori, M. (2004). Evaluation of proximal tooth contact tightness at rest and during clenching. Journal of Oral Rehabilitation, 31(6), 538-545.
- Conroy, J. J. (1994). An investigation of the posterior component of occlusal force (No. AFITCICIA94050).
- Kadam, K. S., & Kurhade, S. S. (2019). Proximal Contact Areas: A Forsaken Facet of Restorative Dentistry. Acta Scientific Dental Sciences, 3(2), 33-34.
- Dörfer, C. E., Von Bethlenfalvy, E. R., Staehle, H. J., & Pioch, T. (2000). Factors influencing proximal dental contact strengths. European Journal of Oral Sciences, 108(5), 368-377.
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!

By: Jeffrey Bonk
Date: June 23, 2021
Featured Digest articles
Insights and advice from Spear Faculty and industry experts



