Bonding to Zirconia: Is It Possible?
Zirconia-based restorative materials were introduced in dentistry almost two decades ago. The first-generation zirconia, Y-TZP, was and still is used as a dental framework material to replace traditional metal. It is a 3-5 mol% yttria-stabilized tetragonal zirconia polycrystalline ceramic. The composition of the material and subsequent mechanical properties, based on its manufacturing, vary. This is true for all generations of zirconia that are available today.
In general, the first-generation material has the highest flexural strength (900–1,200 MPa), fracture toughness (9–10 MPa/m0.5), and fracture resistance (>2000 N). It undergoes transformation toughening, is glass-free, cannot be etched conventionally, and is opaque. Because it’s opaque, it should be used as a framework with a glass ceramic layer to achieve the desired esthetic outcome.
The second-generation Y-TZP is slightly more translucent because it has a decreased alumina content (0.05 wt%). The flexural strength is decreased to 800 to 1000 MPa.
The most recent form of zirconia-based material is the third-generation Y-ZP, a 5–10 mol% yttria-stabilized polycrystalline ceramic with a 10–50% cubic phase that does not undergo transformation toughening. Although it is significantly more translucent, the flexural strength drops to 500–800 MPa. The degree of translucency depends on the manufacturer’s formulation.
With the increase in translucency, it can now be used as a monolithic restorative material. All three generations of materials have similar wear characteristics to enamel, showing virtually no wear.
The questions often posed are: “Can zirconia be bonded?” and “Why would you need to bond?” Bonding any restorative material is indicated when retention needs to be increased. Bonding also improves marginal adaptation, minimizes microleakage, and increases the fracture resistance of the restored tooth and restorative material.1 The indications for bonding a restoration are:
- Compromised resistance and retention form of the preparation
- An overtapered preparation
- Short axial walls
- Partial coverage
- Weaker ceramic materials
After reviewing the literature on bonding to zirconia, the most common method includes airborne-particle abrasion with 50-micron aluminum oxide with application of a primer containing 10-methacryloyloxyethyl dihydrogen phosphate (MDP) or functional methacrylate. Airborne-particle abrasion cleans the surface, reducing organic contaminants that get on the surface during try-in of the restoration. The abrasion increases surface roughness, increasing micromechanical retention.
Alumina remains embedded in the surface, so ultrasonic cleaning is not recommended. The remaining alumina is believed to increase chemical bonding to the adhesive. The air abrasion also increases the surface energy, producing better wettability.
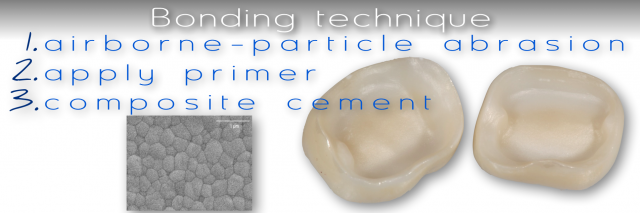
The steps in the bonding technique are2:
- Airborne-particle abrasion
- 50-micron aluminum oxide
- 1–2 bar (15–30 psi) pressure
- 10 mm from the surface, moving in a circular pattern perpendicular to each surface (crowns have five surfaces)
- 5–10 seconds per surface
- Apply MDP or functional methacrylate containing primer/adhesive, following the manufacturer directions
- Examples: Clearfil Ceramic Primary (Kuraray Noritake Dental), Monobond Plus (Ivoclar Vivadent)
- Apply resin cement — dual or autopolymerizing
- Examples: Parvia SA (Kuraray Noritake), Multilink Automix (Ivoclar Vivadent)
Using this protocol, research has shown the bond strength to a first-generation zirconia (Katana HT), third-generation zirconia (Katana UTML), and lithium disilicate (e.max CAD LT) are statistically the same for both short and long-term thermocycling.3
- Katana-HT: 34.22 MPa on Day 1, 28.37 MPa after 150 days
- Katana UTML: 35.04 MPa on Day 1, 25.03 MPa after 150 days
- e.max CAD LT: 35.05 MPa on Day 1, 22.32 MPa after 150 days
Remember, there are two significant variables that must be considered when bonding to zirconia:
- Not all zirconia materials are formulated and manufactured in the same manner, with significant variations in the quality of the zirconia.
- Using a precise clinical technique is essential to establishing the best bond. The literature shows that human error is the most common reason for clinical failures.
References
- Sorensen, J. A., Kang, S. K., & Avera, S. P. (1991). Porcelain-composite interface microleakage with various porcelain surface treatments. Dental Materials, 7(2), 118-123.
- Blatz, M. B., Alvarez, M., Sawyer, K., & Brindis, M. (2016). How to bond zirconia: the APC concept. Compendium of Continuing Education in Dentistry, 37(9), 611-617.
- Kwon, S. J., Lawson, N. C., McLaren, E. E., Nejat, A. H., & Burgess, J. O. (2018). Comparison of the mechanical properties of translucent zirconia and lithium disilicate. The Journal of Prosthetic Dentistry, 120(1), 132-137.
FOUNDATIONS MEMBERSHIP
New Dentist?
This Program Is Just for You!
Spear’s Foundations membership is specifically for dentists in their first 0–5 years of practice. For less than you charge for one crown, get a full year of training that applies to your daily work, including guidance from trusted faculty and support from a community of peers — all for only $599 a year.

By: Robert Winter
Date: November 18, 2018
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


