Loading Protocols for Dental Implants

When a patient presents with an edentulous or soon-to-be edentulous area, the question is often, “How soon can we fix this?”
Patients, and increasingly dentists, are demanding shorter treatment times. Advertisements for “teeth in a day” (or even less) are ubiquitous. In the case of partially edentulous patients — and especially patients who may have not lost a tooth previously — the idea of being without a “permanent” solution can be psychologically challenging. And waiting six months or more? “You’re kidding me, right, doc?”
Certainly, shortened treatment times have many benefits for patients. Yet, if we’re considering osseointegrated implants as the optimal treatment choice for a single missing tooth, we need to have a good understanding of factors that may influence just how soon we can load that implant.
Prosthetic loading
In the early years of osseointegrated implant dentistry, most experts advocated delaying prosthetic loading for three to six months. It was believed that this time frame was sufficient to allow for “stress-free” healing and could compensate for patient-specific factors, as well as not-yet optimized surgical protocols, prosthetic protocols, and implant designs. Although derived empirically, this protocol set the stage for the wide success and acceptance of dental implants as a viable treatment option.
Advances in clinical techniques and innovations in implant surface technology have reduced healing times before loading. Today, options for prosthetic loading can be considered by category.
Conventional loading
Conventional loading is defined as the prosthetic restoration and functional loading of an osseointegrated implant after a healing period of three to six months. As mentioned, this protocol was originally defined for implants with machined surfaces.
Often, but not always, implants following the conventional loading protocol are placed and the surgical site is then closed, requiring a second-stage surgery to “uncover” the implant. This is sometimes described as “delayed loading.”
Immediate loading
At the other end of the spectrum is immediate implant loading. Immediate loading is defined as restoring the implant in occlusal contact within 48 hours of implant placement. Taken to its extreme, the immediately loaded implant could be placed and definitively restored — all within 48 hours.
Immediate loading has shortened the transitional period between implant placement and implant restoration considerably. Benefits for the patient include reduced overall treatment time, reduced number of visits to clinicians, comfort during the healing period, and improved esthetic and phonetic aspects.
Immediate restoration
Immediate restoration, or immediate provisionalization, is similar to immediate loading: The implant is restored within 48 hours, but in this case, the restoration is left out of any functional occlusion.
It’s important to clarify that immediate loading and immediate restoration are independent of immediate implant placement. Although often described together and certainly related, implant placement protocols and implant loading protocols should be considered independently when treatment planning partially and full edentulous patients.
Early loading
Early loading falls temporally between conventional loading and immediate loading. Early loading is defined as the prosthetic loading or utilization of an implant at any time between immediate and conventional loading.
Six to eight weeks of healing is common for early loading protocols, though advances in our understanding of the biologic processes underlying osseointegration and continuing advances in implant surface technology continue to decrease the amount of time required for adequate healing.

Determining loading protocol
To determine which loading protocol is most appropriate for a specific patient situation, several factors must be considered. These factors may be grouped into the same categories as facially generated treatment planning.
Esthetics

Esthetic considerations are often implicated when patients and dentists consider shortened implant loading protocols. Quite understandably, many patients would prefer to have an implant-supported provisional rather than an alternative provisional design. However, rushing to load an implant in an esthetically critical area is counterproductive if the implant fails to osseointegrate. Often, esthetic recovery after an implant failure is more difficult than the original clinical situation.
Conventional and early-loading protocols are more predictable than immediate loading in esthetically critical areas when implants are placed using a delayed approach. When implants are placed immediately after an extraction, there may be some additional value to immediate restoration, especially in cases with thin biotype. Yet, the same benefits of preserving the soft-tissue profile can be achieved using a customized healing abutment.
Function
Occlusal function and parafunctional forces have been implicated in mechanical and possibly biologic complications with implant-supported restorations. As a result, careful assessment of a patient’s wear pattern is recommended. Findings from the occlusal exam can influence the number of implants chosen, their location, and the manner in which an implant restoration is designed. Similarly, occlusal function can influence implant loading protocols.
The application of force to a healing implant may lead to excessive implant movement, which could disturb osseointegration. Occlusal schemes for shortened healing protocols are still being determined. Immediate loading and even immediate restoration should be considered highe- risk protocols in cases of worn dentition where the etiology cannot be distinguished or occlusion cannot be managed adequately.
Structure
Determining the anticipated restorative outcome is crucial to determine the most optimal implant position. Once the optimal position has been determined, the potential site may be evaluated from a surgical perspective. Will it need to be augmented horizontally? Vertically? Would soft-tissue augmentation help mask bony resorption that followed a previous tooth extraction?
Many authors suggest avoiding immediate and early loading in clinical situations that required significant grafting, even in cases where the grafting was completed before the implant being placed.

Biology
Successful osseointegration depends on several factors:
- Suitability of the implant material
- Careful site preparation
- Adequate stabilization of the implant
Of these three factors, adequate stabilization of the implant is the most critical to selecting a loading protocol. Loading protocols should be viewed as dependent on, among the other factors described here, two distinct processes: primary and secondary implant stabilization.
Understanding these concepts helps in understanding why different loading protocols could be used, or should be avoided, depending on the clinical situation.
As an implant is placed into a prepared osteotomy, parts of the implant body and threads come into direct contact with bone. This primary bone contact provides primary stability. Because the stabilization provided is mechanical in nature, this is often referred to as “mechanical stability.”
As healing progresses, the original bone around the implant surface remodels and areas of new bone emerge at the implant surface. The remodeled bone contact and new bone contact result in secondary or biologic stability. Biologic stability predominates at later healing times and the influence of the primary stability decreases over time.
Bone healing resulting in biologic stability can be disturbed if the mechanical stability is inadequate. Movement of the implant above a physiologic threshold is thought to disturb the adjacent tissues and vascular structures, eventually resulting in failed osseointegration. As a result, when considering shortened loading protocols, clinicians should focus on the:
- Amount of primary bone contact/primary stability
- Quantity and quality of bone at the implant site
- Pace of bone formation around the implant
In the case of inadequate primary stability, surgeons may elect to increase the diameter of the implant being placed or avoid immediate loading. When existing bone of high quality and quantity is found and when other factors are favorable, immediate loading of the implant may be possible.
Bone quality and bone quantity are related to different areas in the mouth. An implant site in the anterior mandible is often a better candidate for a shortened loading protocol when compared to a site in the posterior maxilla. In cases where implants are placed in type IV bone or heavily grafted bone, conventional loading protocol may be beneficial.
The pace of bone formation may be favorably influenced by advances in, among other things, implant surface technology. As a result, early loading is becoming routinely possible. Depending on the specific surface technology, early loading may be accomplished in as little as three weeks.
Clinical case
This case illustrates some of the risks and dangers involved with a shortened loading protocol. Here, the patient presented with a nonrestorable maxillary left central incisor and would like to have an implant placed.
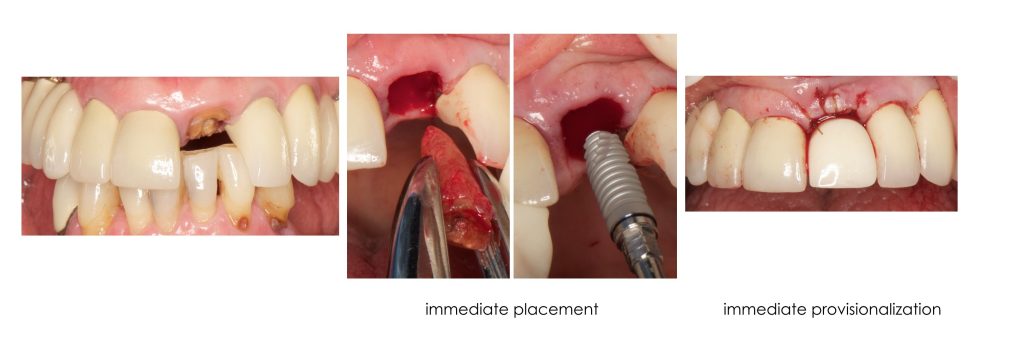
- Esthetics: The implant site is in the esthetic zone.
- Function: The patient lacks posterior support, deep vertical overlap (overbite) present.
- Structure: Additional teeth require restoration due to dental caries.
- Biology: Thin biotype.
The nonrestorable tooth was extracted and an implant placed into the socket. The implant was immediately restored with a screw-retained provisional.
At a three-week postoperative visit, the patient complained of mobility with the implant restoration. The implant/provisional crown complex was removed by hand.

Conclusion
When using modern dental implants, conventional and early loading protocols are both well documented and predictable. Interdisciplinary teams may choose a longer healing period in sites that are compromised or in patients in which healing is expected to be altered.
Immediate loading in partially edentulous patients is possible in select cases, but the evidence for successful outcomes is less extensive.
Many patients are eager to have their treatment completed as rapidly as possible. Individual dentists and interdisciplinary teams are reminded that immediate loading has increased risk of implant failure and should be used in esthetically critical areas only after careful consideration of the benefits, risks and alternatives.
References
- Rowan M, Lee D, Pi-Anfruns J, Shiffler, P, Aghaloo, T, Moy P. Mechanical versus biological stability of immediate and delayed implant placement using resonance frequency analysis. Journal of Oral and Maxillofacial Surgery.
- Albrektsson T, Wennerberg, A. (2013) The Science of Osseointegration. In Zarb, Hobkirk, Eckert, Jacob. Prosthodontic Treatment for Edentulous Patients. St. Louis: Elsevier.
- Beumer J, Faulkner R, Shah K, Moy P. (2015) Fundamentals of Implant Dentistry. Quintessence.
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!

By: Darin Dichter
Date: August 13, 2018
Featured Digest articles
Insights and advice from Spear Faculty and industry experts