Managing the Forces: Occlusal Considerations With Implants
Dental implants have become a standard option for replacing teeth, but there are differences between a natural tooth and a dental implant. For instance, as with natural teeth, a dental implant can acquire bone loss (peri-implantitis), but unlike a natural tooth, it is more susceptible to occlusal overload — the main reason being the difference in the interface to the alveolus. In this article, we will look at occlusal considerations clinicians must consider with implants.
Periodontal ligament vs. osseointegration
So, what is that difference in the interface to the alveolus? It starts with the fact that the periodontal ligament (PDL) connects a natural tooth to the alveolus, while a dental implant is directly attached to the bone through osseointegration. The presence of the PDL provides increased protection against occlusal overload by sending information to the central nervous system, which provides feedback to the elevator muscles that elicit a protective reflex to reduce occlusal forces.
In addition, the PDL offers additional protection by absorbing pressure when heavy occlusal forces are applied to the tooth. A natural tooth can be displaced 25–100 µm in the axial direction and 56–108 µm horizontally, compared with a dental implant, which can only be displaced 3–5 µm axially and 10–50 µm horizontally. The PDL also allows the tooth to adapt to excessive forces through intrusion or rotation and by distributing the load along the entire root surface. In contrast, because a dental implant is connected directly to the bone, it does not have the same adaptive capabilities. Thus, if an implant is subjected to similar forces, the load is concentrated at the crestal bone, increasing the susceptibility to irreversible bone loss.

Mutually protected occlusion
When restoring a dental implant, the restorative dentist must evaluate the risk factors and develop an occlusal relationship that minimizes the risk of occlusal overload. For example, an 80-year-old woman will typically generate fewer occlusal forces than a 30-year-old male bruxer.
Because the risk factors increase in patients with a history of occlusal diseases — such as parafunctional habits, bruxism, steep cusp inclines, and poor occlusal distribution — implant occlusion must be managed differently. While the location and number of dental implants play a role in force distribution, the restorative dentist must develop an occlusal scheme that minimizes implant complications such as bone loss, prosthesis fracture, screw loosening, and implant failure.
Like a natural tooth, an implant restoration needs equal and bilateral occlusal contact to protect the implant fixture and the restoration. However, because of the differences between a tooth and an implant, there are variations in how the restorative dentist manages the occlusion when restoring a dental implant. The primary objective is to develop an occlusion in which the forces on the dental implant remain below the physiological limits of the surrounding bone. A mutually protected occlusal scheme protects the dental implant from overload by sequencing the contacts between the implant restoration, adjacent teeth, and the opposing arch.
Static occlusion
When delivering an implant restoration, the restoring dentist must recognize the physiologic differences between a dental implant, a natural tooth, and the surrounding bone. Because a dental implant cannot adapt under heavy occlusal forces, it will be introduced to premature contacts when the tooth-borne and implant restoration are adjusted similarly. A mutually protected occlusal scheme will protect the implant in vertical and lateral movements to avoid the negative consequences of early contact with the dental implant.
Steps to adjust the static occlusion:
- Evaluate the occlusion on the natural dentition before restoring the implant restoration.
- Evaluate the occlusion on the implant crown by having the patient tap lightly on articulating paper.
- Adjust the implant crown so the shimstock barely slides between the implant restoration and the opposing arch while the patient bites lightly.
- Instruct the patient to squeeze their teeth together tightly to ensure equal contact with the adjacent natural teeth and the implant restoration.
- Verify that the contact is directed down the long axis of the dental implant.

Dynamic occlusion
Once the static occlusion is established, it is essential to adjust the dynamic occlusion to eliminate or share the lateral contacts on the implant restoration. This will reduce the shear forces generated on the implant fixture when excessive lateral forces are placed on the implant restoration. While adjusting posterior teeth with adjacent natural teeth, the implant restoration must be free of working or balancing interferences. If multiple implants replace an entire segment, the restoration should be splinted to distribute the lateral forces between the implants.
Canine guidance
In the natural dentition, canine guidance is developed to decrease muscle forces, but when a single implant replaces a cuspid, canine guidance should be avoided. The neighboring premolar and lateral incisor should share the load during excursive movements, adjusting the dynamic occlusion using the same timing previously discussed for the static occlusion and ensuring the excursive forces are shared between the cuspid and adjacent teeth.
Prosthesis design
The restoration design can also contribute to unwanted excessive forces on the implant fixture. The design of a posterior restoration should incorporate an occlusal table with a flat contact area perpendicular to the implant body, directing the forces down the long axis of the fixture. Increasing the leeway space and designing the restoration with cuspal inclines less than the natural dentition will account for the mobility differences between a tooth and implant and eliminate working and balancing interferences.
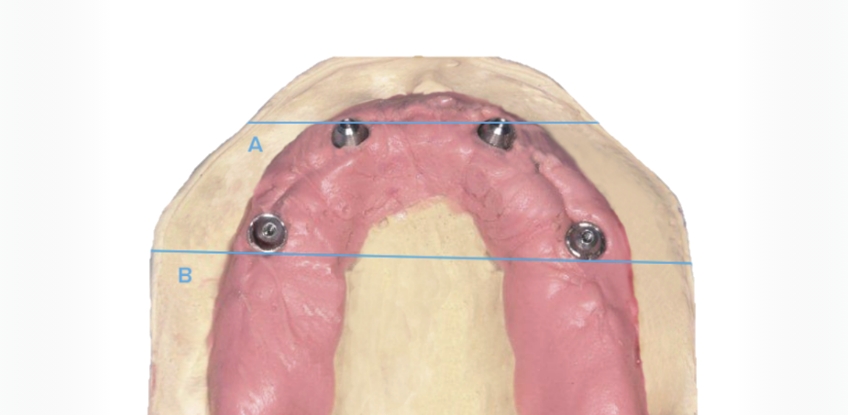
It is customary practice to use implants to replace an edentulous arch. Cantilevers are used to add posterior teeth beyond the maxillary sinuses or to avoid the inferior alveolar nerve to increase the restoration’s biting surface and provide a complete dentition. When a cantilever is designed in the restoration, it should not be greater than 15 mm, or 1.5 times the A-P spread of the anterior and posterior implants. If a cantilever exceeds that recommended length, the distal implant can be subjected to excessive shear forces, and there is an increased risk of prosthesis breakage.
The prosthesis design is only one factor that decreases the risk to the implants and restorations under excessive forces. To develop a patient-specific treatment plan, each patient must be evaluated before implant placement. Additional implants may be needed, and the prosthesis design becomes more critical for the long-term stability of the restoration when there are increased occlusal risk factors.
Managing occlusal considerations with implants
Recognizing the differences and managing occlusal considerations between a tooth and a dental implant is essential for implant fixture and restoration success. All these factors reduce the risk of complications and result in a better outcome for your patient.
References
- Misch CE. (2005). Dental Implant Prosthetics (pp. 472–507). Elsevier Mosby.
- Gross MD. (2008). Occlusion in implant dentistry. A review of the literature of prosthetic determinants and current concepts. Australian Dental Journal, 53, S60–S68.
- Sheridan RA, Decker AM, Plonka AB, Wang HL. (2016). The role of occlusion in implant therapy: A comprehensive updated review. Implant Dentistry, 25(6), 829–838.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Curt Ringhofer
Date: October 26, 2023
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


