The Importance of Occlusal Analysis in Condylar Seating
By Darin Dichter on May 26, 2022 | commentsRestoring patients to their existing bite, or the position of maximum intercuspation (MIP), is the most common way dental patients are treated in North America and the world. While clinicians often prefer this approach due to its apparent simplicity, there are clinical scenarios that demand evaluation of the tooth-to-tooth contacts that occur when the condyles seat, such as occlusal analysis. In addition, there are clinical circumstances in which the dentistry proposed for a patient may destabilize the existing MIP and a new occlusion must be established, such as a full arch of restorative dentistry.
To proceed in either case, the clinician must evaluate the patient's ability to achieve and tolerate a seated condylar position and record the occlusal relationship in this mandibular (condylar) position.

Clinically, options for seating condyles and making occlusal records in this position include:
- Bimanual manipulation
- Anterior deprogrammers, such as a Lucia jig or leaf gauge (Fig. 1)
- Another type of appliance
Interestingly, the literature suggests no one technique is more accurate than another. Regardless of the selected technique, there are scenarios when the clinician may experience difficulties in achieving a seated condylar position. Common problems that may prevent condylar seating include:
- Muscles have not released
- Problem in temporomandibular joint
- Posterior tooth contact
While muscle or joint issues can be identified during a clinical exam, posterior tooth contacts that prevent the condyles from seating can be challenging to identify. The following case demonstrates an example of posterior tooth contacts preventing condylar seating.
Re-establishing the occlusal scheme
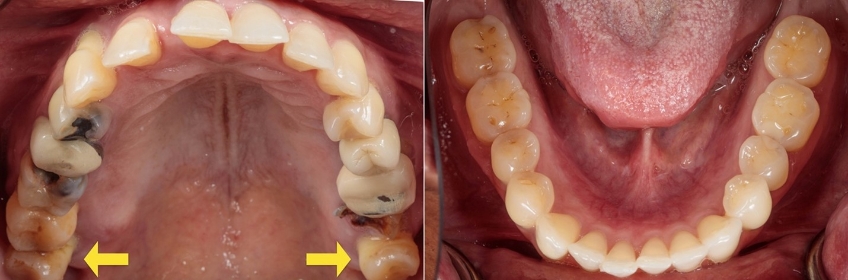
A periodontist referred a 51-year-old female patient for evaluation of periodontally hopeless maxillary dentition. A screening exam revealed her dentate with a reasonably intact mandibular dentition but severe structural and biologic compromise to the maxillary arch, requiring re-establishment of the entire occlusal scheme [Fig. 2].
The patient was clinically missing the mandibular third molars; however, both third molars were present in the maxilla. In addition, a sizable portion of the clinical crown of the upper left second molar was missing [Fig. 3].

Clinically, both maxillary third molars were mobile, compressible, and appeared to have erupted beyond the occlusal plane. This feature is more readily apparent in the reconstructed orthopantomogram [Fig. 4]. The maxillary third molar tooth position did not prevent the patient from closing into MIP.
The patient and the referring clinician both believed the maxillary teeth to be hopeless and were interested in restorative options to replace the soon-to-be missing teeth.
To better assess the existing condition, an occlusal analysis was prescribed. A digital impression of both arches was made using a CEREC Primescan (Dentsply Sirona). Due to the degree of mobility, the imaging of the upper right third molar was incomplete despite multiple attempts [Fig. 5, 6].



To proceed with the indirect occlusal analysis the desired occlusal relationship to record with the buccal bite is at a seated condylar position. Further, if this patient is to proceed with a full arch reconstruction (tooth- or implant-retained) treating in a seated condylar position provides a significant degree of improved functional predictability and convenience. In either case, the patient must be able to have their condyles seated and be able to tolerate the occlusal load in that position.
In this case, when asked to bite into MIP the patient expressed no problems and could do so repeatedly (Fig. 7, left). However, when a deprogrammer (leaf gauge) was introduced to allow the condyles to seat, it became evident that even at the full thickness, the leaf gauge was insufficient to clear the occlusal contacts at the maxillary third molars (Fig. 7, right). As a result, in this case, the leaf gauge was inadequate for seating this patient's condyles due to the posterior tooth contact. Importantly, it is unlikely that any other mode of seating condyles would have been successful in this scenario.
The key to seating the condyles, in this case, is solving the posterior tooth contact problem. Since the maxillary third molars are so far out of position and considered periodontally hopeless, it was suggested to the patient to have them removed, along with the structurally hopeless maxillary left second molars.

Surprisingly, while the maxillary posterior teeth created a significant challenge to achieving and recording a seated condylar position for this patient, the aberrant tooth position did not appear to restrict or significantly alter the mandibular movements into or away from maximum intercuspation. The patient was unaware her posterior teeth were creating any functional problems. On the surface, this may sound like good news. Yet, this could have lessened the likelihood that the occlusal discrepancy would be noticed by a clinician and the inaccurate occlusal record accepted as accurate.



Occlusal analysis in a fully seated condylar position
While a significant volume of dentistry is completed utilizing the patient's existing bite, there are certain clinical circumstances that require an occlusal analysis in a fully seated condylar position or even treated to that position where a new occlusal scheme could be established. Problems with seating condyles are typically related to incomplete muscle release, TM joint problems, or posterior tooth contact. When such a problem exists, clinicians must recognize the situation and treat it accordingly or risk introducing a significant error into the functional aspect of the case planning.
Darin Dichter, D.M.D., is a member of Spear Resident Faculty.
References
- Ferro, K. J., Morgano, S. M., Driscoll, C. F., Freilich, M. A., Guckes, A. D., Knoernschild, K. L., ... & Twain, M. (2017). The Glossary of Prosthodontic Terms.
- McKee, J. R. (2005). Comparing condylar positions achieved through bimanual manipulation to condylar positions achieved through masticatory muscle contraction against an anterior deprogrammer: a pilot study. The Journal of Prosthetic Dentistry, 94(4), 389-393.
- Radu, M., Radu, D., & Abboud, M. (2020). Digital recording of a conventionally determined centric relation: a technique using an intraoral scanner. The Journal of Prosthetic Dentistry, 123(2), 228-231.