Some Questions I’ve Been Asked About Occlusion Over the Years, Part 2
In my first “Questions I’ve Been Asked About Occlusion” article, back in November, I answered some of the reoccurring questions I have been asked over the years about occlusion. Here I will answer some more. I hope you find my answers are helpful.
What Kind of Bite Splint Do You Make?
When I am asked this question, my response is always the same — it depends. Tell me the diagnosis and what you are trying to accomplish with the bite splint, and then I can tell you what bite splint to use.
Many I speak with use one “go to” bite splint style for everyone. Impressions are taken and sent to the lab with a script for a maxillary hard/soft bite splint. No facebow or record of the TMJ position and sometimes no bite registration. Is it a seated condylar position or a maximum intercuspation bite? So, who is really treating the patient? The dentist or the lab tech?
When the bite splint is inserted the doctor asks the patient, “How does it feel?” In my experience a patient generally doesn’t know how to respond to this question, so I don’t ask it at this time.
Like every other aspect of health care, to treat someone we first gather data, develop a diagnosis, and treat that diagnosis. In Spear’s occlusion workshop we teach how to evaluate the temporomandibular joint and muscles. Since most TMD patients have extracapsular problems, Spear teaches how to make and adjust an anterior sectional appliance to help muscles relax.
Many times, post-ortho, I will make a retainer for the maxilla with an anterior platform and a mandibular retainer with an anterior stylus to allow retention of tooth position and free and easy movement of the mandible with no posterior interference, which is also taught in the Occlusion in Clinical Practice workshop.
However, a sectional appliance doesn’t give a patient the experience of comfortable occlusion. Most appliances I make are full arch appliances equilibrated several times over several months to assure a mutually protected occlusion in a fully seated condylar position, which happens to be taught in the Advanced Occlusion workshop.

So, when do I ask the patient how it feels? When I insert any bite splint, I tell them it is designed to fit tightly and I ask them, “Are there any spots that are so tight it’s sore?” I occasionally adjust a minor amount.
The purpose of my question is to inform the patient that the appliance is supposed to fit snugly. When I adjust an anterior sectional splint to where I have the contacts I want and smooth excursions then I ask, “Can you feel the front teeth hitting evenly or is there a spot that feels a bit harder?”
Sometimes a small rubber wheel adjustment is needed. Also, as they move through excursions, I have my finger on their chin to feel what they feel. If I feel any roughness or bumps, I point it out, adjust it and ask, “Does that feel smooth to you? Do you feel any other bumps?”
I advise to ask questions that will guide you to improve the function of your treatment. When I insert and fully adjust a full-arch splint, I tell my patient, “I want you to feel all of your back teeth hitting at the same time and with even pressure. When you move your jaw in any position, I want only your front teeth to be touching and your back teeth not touching at all. Is that what you feel?”
Remember there is no magic in the plastic. The magic is with good data collection, a good diagnosis, and good care.
Won’t Most People Benefit From a Nightguard?
Too many times I have seen a dentist look at a wear pattern on a tooth and just assume it was from the patient grinding their teeth. Then the patient is promptly given the standard magical nightguard that helps everyone.
On my new patient health/dental questionnaire there is a question that reads, “Do you grind your teeth?” If the “yes” box is checked I ask the patient, “How do you know you grind your teeth?” The most common answer I hear is, “My dentist told me.”
The answer to this question is again — it depends.
A patient will benefit from a bite splint/nightguard if, in fact, it addresses the correct diagnosis. Sometimes we get lucky. Today, we know the airway can be a contributing factor to parafunction. Will the bite splint open the oral volume to allow more room for the tongue and thus less interrupted sleep? Will the bite splint change the tooth stimulation and thus muscle engrams? Does your patient feel better, or just wear it because the doctor told them so?
I would encourage you to ask every patient you have made a bite splint/nightguard for if they are wearing it as prescribed. The result may be surprising. If they are not wearing it find out why? Was it the wrong splint or the wrong diagnosis?
Most of my patients do not have a bite splint. Those who do, wear it regularly and bring it with them to hygiene checks so it can be evaluated and cleaned.
Do You Treat All Your Cases in Centric Relation?
Centric relation (fully seated condylar position) doesn’t matter except when it does. Most patients we treat do not have a maximum intercuspation position of their teeth and a fully seated condylar position coexisting. Most involve just a few teeth and our intent is not to alter their occlusion and joint position. The good news is in most cases things work out well.
When I am doing a comprehensive care case, I want to work from a fully seated condylar position. Why?
If I have a centric relation position that I can transfer to an articulator, then I can duplicate all the movements my patient can make and see the effects on their dentition. This allows me to modify or build a result that has a very good level of predictability.

Please note that a comprehensive care case does not mean I’m crowning every tooth in the head. It means I’m looking at all the functioning systems and addressing what needs attention. If my evaluation reveals a healthy situation, then there is no need to alter what is working well.
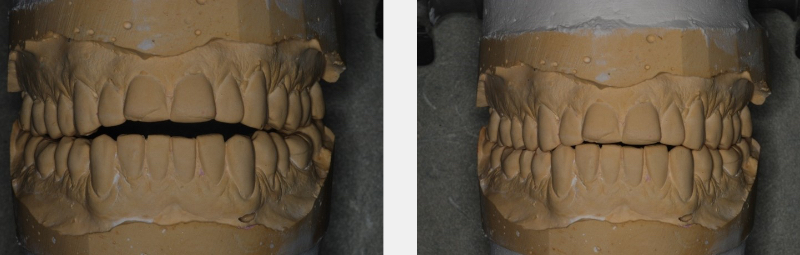
I also want to treat my ortho cases in centric relation. I believe tooth movement is a full-mouth rehab, though I may not be doing very much restorative, I want to know the condyle is seated so when the ortho is completed the post-ortho equilibration has a fully seated condylar position and a maximum intercuspation position coexisting.
Whether the ortho is pre-prosthetic or an adolescent with a developing occlusion, having a fully seated condylar position allows for a more predictable long-term, stable result.
Does Everyone Need to be Equilibrated?
In dentistry, as in life, decisions are not black and white. Since every patient is different, the care they receive should be customized as well.
Maybe this article should have been titled “It Depends.” Everyone does not need to be equilibrated. Many will function and adapt in a non-equilibrated world. But when a need for equilibration is identified, then it should be done with the condyle in a seated position. Instead of fixing a tooth, treat the patient. Figure out why the problem occurred.
Understanding function, which has to do with the relationship and harmony of TMJs, muscles, teeth (occlusion) and airway, will make your dentistry more predictable and your dental life less stressful.
While there is no specific cookbook with yes or no answers, your journey in understanding dentistry is a lifelong commitment. Don’t your patients deserve it? Don’t you deserve it?
Good luck on your journey, may it lead you to where you want to go.
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Carl Steinberg
Date: January 8, 2021
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


