FPDs Vs. Implants Part II: How Do FPDs Most Often Fail?
By Frank Spear on February 10, 2019 |It is very common to hear clinicians speak about their anxiety of using FPDs - especially if the FPD has more than one pontic - but I don’t often hear people say specifically how they believe the FPD will fail.
What I do hear are statements like, “I don’t think those teeth can support an FPD that long,” or that doing that FPD will just be wasting the patient's money because it will fail. I also hear that it’d be better to just take out the questionable abutments, place implants and be done with it – which is definitely true in some cases, but not all. Not to mention the patient limitations we face in terms of their ability to afford some of our more heroic treatment plans.
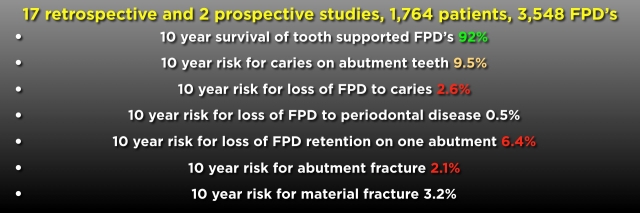
What I want to do in part two of this ongoing series on FPDs vs implants is look specifically at literature that has evaluated the specific types of complications that occur in FPDs, along with the incidence with which they occur. The specific article we will look at is a systematic review from the UK that used 19 papers covering 1,764 patients and 3,548 FPDs, a significant database of information.

Next, I’ll show a slide of the findings of this review, which lists the complications seen over 10 years for all 3,548 FPDs. It also lists the incidence of the complication.
I have color-coded the results to make them easier to understand.
The green text is the 92 percent 10-year survival rate that is very close to the article I used in part one of this series, and is equal to the 10-year results for implant-supported single crowns or implant-supported FPDs.
The cantaloupe color is the incidence of recurrent caries on the abutments over 10 years. This percentage shows caries that did not result in the loss of the FPD, but simply caries that required a restoration.
The red text shows the three areas that resulted in loss of the FPDs: loss of retention on one abutment (6.4 percent), abutment fracture (2.1 percent) and deep caries (2.6 percent). Periodontal disease was not a significant issue in this review, and material failure (e.g. porcelain fracture or chipping) occurred 3.2 percent of the time.
It is interesting to note that this review did not list the incidence of endodontic therapy required after placing an FPD, as not all the included articles used had assessed it. The article “Analysis of Endodontic Complications Following Fixed Prosthodontic Rehabilitation,” cited below, looked specifically at the incidence of endodontics following FPD placement in 524 patients with 1,663 abutment teeth, and found it to be 6.3 percent three years post-FPD placement.
The take-home for me from the literature presented is that the loss of retention from one abutment, (or fracture of an abutment) in addition to deep caries, will be the most likely modes of FPD failure. The loss of retention and prep fracture are related to a few things: excess occlusal loading, structurally-weak abutments (such as those with endo), a post-core, no ferrule, and inadequate resistance and retention form in the tooth preparation (such as an excessively short or tapered preparation).
If the patient presents with a low caries history, manageable occlusion and structurally-acceptable vital abutment teeth, FPDs can prove to very acceptable long-term. The patient below is an example.




References
Int J Prosthodont. 2016 Nov/Dec;29(6):565-569. Analysis of Endodontic Complications Following Fixed Prosthodontic Rehabilitation. Uzgur Z, Uzgur R, Çolak H, Ercan E, Dallı M.
(If you enjoyed this article, click here for more by Dr. Frank Spear.)