With evolution comes turbulence caused by change. Spear Education is taking a leadership role in evaluating airway dynamics and promoting resolution strategies.

In establishing a foundation for this revolution, it has become obvious that airway problems go beyond sleep and apnea. One issue dentists face is the focus of medicine on disease rather than prevention. The traditional sleep study focuses on quantifying extreme disease rather than isolating airway problems before they become deadly.
Obstructive sleep apnea (OSA) diagnosis and severity is based on the number of apnea and hypopnea events per hour of sleep. Apnea is defined as a 90 percent or greater reduction in airflow lasting 10 seconds or longer with an associated 4 percent oxygen desaturation.
Hypopnea has multiple definitions. This creates confusion amongst sleep laboratories and airway researchers.
Limitations to working definitions of hypopnea
In 1999, the American Academy of Sleep Medicine (AASM) defined a hypopnea as a reduction of airflow with a 3 percent reduction in oxyhemoglobin saturation or an arousal. In 2007, the AASM provided two alternative definitions:
- a 30 percent reduction in airflow with a 4 percent reduction in SpO2, or
- a 50 percent reduction in airflow with either a 3 percent decrease of oxyhemoglobin saturation or an event-related arousal.
The former requires a higher level of desaturation and eliminates the arousal, making it more difficult to attain. That definition was adopted by Medicare for reimbursement criteria and thus became the more accepted definition.
The impact of the choice of a more stringent metric could absolutely impact the claim of causality for the health-related consequences of OSA. The Medicare definition could also ignore the early disease detection of the patients that could be prevented from obtaining airway-related illness.
Additionally, because many of the dental signs and symptoms are related to minor inspiratory limitations, they will not be diagnosed during a typical sleep study. This prevents an important link between dentistry and medicine.
The magnitude of the impact of Medicare's choice of definition was examined.1
Findings from the Sleep Heart Health Study
The Sleep Heart Health Study is a prospective study designed to evaluate the link between OSA and cardiovascular disease.
In-home polysomnograms (PSG) were completed on 6,441 subjects. The PSGs were scored for hypopneas in three different ways. All classifications required a 30 percent reduction in airflow. That reduction was paired with either:
- a 4 percent or greater desaturation,
- a 3 percent or greater desaturation, or
- a 3 percent or greater desaturation or an event-related arousal.
The AASM Sleep Apnea Definitions Task Force proposed the later definition in 2012.
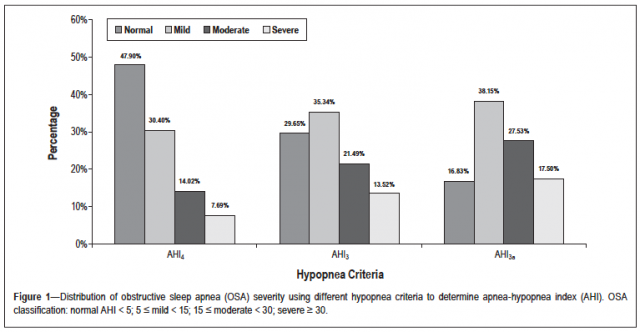
As you might expect, the method of scoring significantly altered the prevalence and severity of apnea. Lower levels of apnea are most sensitive to the change in definition, highlighting the claim that many more patients at the lower levels would be diagnosed and treated with the new criteria.
The inclusion of arousals detected the more sympathetically active patients that dental practitioners describe routinely as the bruxer, clencher and TMD patient. Utilizing the Medicare criteria, 47.90 percent of the patients were diagnosed as normal. That number fell to 16.83 percent with the Task Force definition of hypopnea.
The number of patients classified as severe also increased from 7.69 percent to 17.50 percent. These severe patients could qualify for additional medical assistance, including orthognathic surgery on some insurance plans.
Lastly, the Task Force definition does not include inspiratory flow limitations without arousals that have been shown to set the stage for future airway compromise. Their inclusion would further reduce the normal subjects.
The study also underscores the point that the vast majority of our cardiovascular patients have pre-existing obstructive breathing and deserve monitoring. Dentistry can play an important role in screening (and many times, treating) these types of patients.
Jeff Rouse, D.D.S., Spear Faculty and Contributing Author
References
1. Ho V, Crainiceanu C, Punjabi N, Redline S, Gottlieb D. Calibration model for apnea-hypopnea indices: Impact of alternative criteria for Hypopneas. Sleep 2015;38:1887-1892.