As If the Debate About Centric Relation Wasn’t Enough: Part I
By Kevin Kwiecien on July 23, 2015 | Do you remember the way it felt when you finally understood the difference between their, there and they’re? What about being able to distinguish between to, too and two?
Do you remember the way it felt when you finally understood the difference between their, there and they’re? What about being able to distinguish between to, too and two?
You probably let out a sigh of relief, stored it away as foundational learning and assumed you would never have to question it again. To a certain extent, that is the way I finally felt after years and years of learning and re-learning TMJ anatomy, muscle function, anterior guidance, location of posterior stops and the concept and use of centric relation in clinical practice. I trusted it, philosophically and practically.
My goal for every case that I mounted for evaluation or treatment planning was to identify the steps it would take to restore my patient to that position. Even if it wasn’t appropriate for that patient, I always wanted to discuss the optimal plan and help them see the benefit of this wonderful orthopedically-stable position that most human bodies would appreciate. Similarly, the goals of almost all of my occlusal appliances was to start as close to – and continue to move towards – a fully seated condylar position, release the lateral pterygoid and create the most orthopedically-stable position possible when they were wearing the appliance.
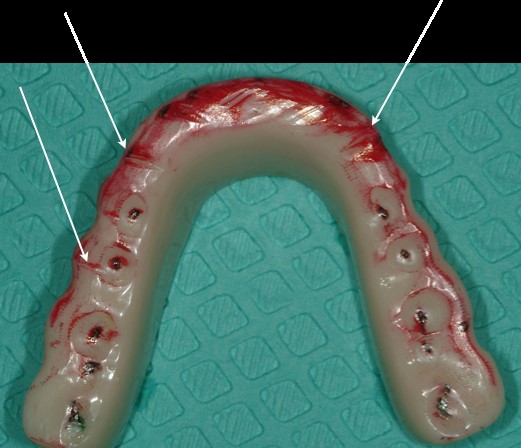
Similar to the intentions of a band-aid or a crutch, wearing the appliance is better than continued disharmony or breakdown, right? But why were some of my patients still wearing deep grooves into the appliances and still having some muscle tenderness? (Figure 1)
I Did Some Research
I trusted what I had learned from my time with Frank Spear, Gary DeWood, Steve Ratcliff, Sam Higdon and so many other brilliant clinicians and educators – so I needed to prove to myself that it was still right. Being the dental nerd that I am, I did some research. I found that I was actually not the first to experience this. Thank goodness I wasn’t alone.
A well-done article from 2009, comparing the efficacy of occlusal splints, documented that "occlusal stability depends on the physical status of the muscles and may be influenced by physical and mental stress." That made complete sense to me. Psychological factors can certainly affect muscle tension and behavior, but I felt fairly confident that my patients were within a normal range. The article also noted "the difference between CR and MI should be considered. When there are large differences between these positions, use of CR may be more favorable." (1) My confidence was high but I wondered what I was missing – or what psychological factors I could be missing.
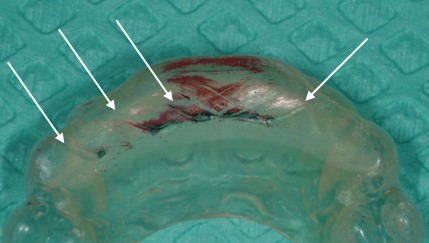
As so many dentists have learned during their journey with Spear Education, an anterior bite plane can have a positive and dramatic effect quieting the muscles, so I tested that theory with several of my patients that were wearing grooves into the full-ach appliances. (Figure 2)

I knew that this would negate any possibility of small excursive posterior interferences from activating the large muscles of mastication. Would you believe that they were still wearing some significant grooves in these appliances? (Figure 3)
And Then I Did Some More Research
As I looked deeper into this, I found a 2007 article that documented similar findings; it concluded that "a recent study was unable to demonstrate a significant difference between the NTI and conventional oral splint in treatment efficacy." It also concluded that "the possible pain- or discomfort-relieving effect of an NTI or OS (occlusal splint) has been demonstrated in some, but not all, studies and suggests a possible involvement of other mechanisms." (2)
Other mechanisms? My curiosity was piqued, so I resorted to taking a few steps back by reviewing current literature on bruxism. In doing so, I stumbled upon many articles that had the name Gilles Lavigne as the primary or contributing author.
One in particular, had a title that a simple-minded person like me could appreciate, “Bruxism physiology and pathology: an overview for clinicians.” It clearly documented that sleep bruxism was recently classified as a “sleep-related movement disorder” and that sleep bruxism is "secondary to sleep-related micro-arousals." (3) The study notes that bruxism "peaks in the minutes before rapid eye movement sleep, which suggests that some mechanism related to sleep stage transition exerts an influence."
Am I Making My Patients Worse?
This all made sense to me and I was feeling that sigh of relief coming on, knowing that I was dealing with something out of my control. But then I read an article that I wish I would have accidently skipped – but the title, “Aggravation of respiratory disturbances by the use of an occlusal splint in apneic patients: A pilot study,” jumped out at me like a bad dream during an episode of severe bruxism. The study actually identified four patients that experienced an aggravation in the apnea diagnosis category on the night they used the splint. It also suggested that the use of an occlusal splint is associated with the risk of aggravation of respiratory disturbances. The authors further suggested that it may be relevant for clinicians to question patients about snoring and sleep apnea when recommending an occlusal splint.(4)
This was disturbing news to say the least, since I had delivered hundreds of appliances for patients with a myriad of symptoms ranging from: muscle pain, joint instability, restoration protection, and nighttime bruxism. How many of those patients were like the four patients in the pilot study? Was I making my patients worse by helping them find comfort in an orthopedically-stable position with the condyles seated and lateral pterygoids relaxed? Were those four patients wearing notches into the appliances that were well-made, delivered, and properly adjusted for them just like my patients?
As with most aspects in dentistry, there is rarely a clear answer. Regardless, it cannot be ignored by me or any other dentist delivering appliances in centric relation – especially for patients with bruxism or that continue to quickly wear marks into a well-adjusted appliance. In the next article, I will discuss the ambiguity surrounding this dilemma and the steps that we can all take to help our patients make healthy decisions and live a health-centered life.
Kevin Kwiecien, D.M.D., M.S., Spear Faculty and Contributing Author
References
- J Appl Oral Sci. 2009;17(1):32-8, Comparitive Evaluation of the Efficacy of Occlusal Splints Fabricated in Centric Relation or Maximum Intercuspation in Temporomandibular Patients, Marcelo Matida HAMATA1, Paulo Renato Junqueira ZUIM2, Alicio Rosalino GARCIA2
- Journal of Oral Rehabilitation 2007 34; 105–111, Effect of a nociceptive trigeminal inhibitory splint on electromyographic activity in jaw closing muscles during sleep, L . Baad-Hansen , F . Jadidi , E Castrillon , P . B . Thomsen & P Svensson
- J Oral Rehabil. 2008 Jul;35(7):476-94. Bruxism physiology and pathology: an overview for clinicians, Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K.
- Int J Prosthodont. 2004 Jul-Aug;17(4):447-53. Aggravation of respiratory disturbances by the use of an occlusal splint in apneic patients: a pilot study. Gagnon Y, Mayer P, Morisson F, Rompré PH, Lavigne GJ