The Two Rules of Subgingival Margin Placement
Subgingival margin placement is necessary for several reasons: to hide the margin on a discolored tooth; to hide the margin when a more opaque restoration is placed; to chase old restorations or decay; or sometimes to increase the amount of tooth structure for the restoration.
When treatment-planning for subgingival margin placement, you must be aware of your patient’s sulcus depth. Knowing how to prep your patient’s teeth and where to place the gingival margins is essential if you want a predictable and esthetic result. I personally have two rules when it comes to subgingival margin placement:
Rule 1: Probing depth ≤ 1.5 mm
If probing depth is 1.5 mm or less, extend 0.5–0.7 mm below tissue.
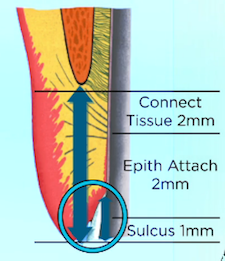
When patients have less than 1.5 mm of sulcus depth, you have a minimal risk of recession. We know the tissue won’t recede into the biologic attachment, so placing the margin more than 0.5–0.7 mm is unnecessary to hide the margin in shallow sulcus patients. In fact, even if you cut off all the tissue to bone, you will get regrowth of the tissue to re-create the attachment and at least a 1 mm sulcus.
That means in these patients, the risk in prepping subgingival margins is going too deep and violating the attachment, which can result in inflammation. My rule in these cases is always to extend 0.5–0.7 mm below tissue, but not any deeper, to avoid prepping too far into the attachment.
Rule 2: Probing depth > 1.5 mm
If the probing depth is greater than 1.5 mm, go half the depth of the sulcus below tissue, or perform a gingivectomy if possible to reduce the sulcus depth and reduce the risk of recession.
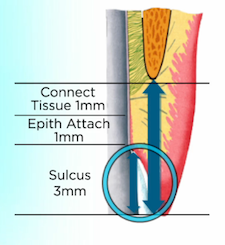
For cases that have a deeper sulcus, the risk of recession can be high. The reason there is a greater risk of recession is due to the unattached tissue. When there is 3–4 mm of sulcus depth, it means there is 3–4 mm of unattached tissue above the biologic attachment. It may be a stable tissue level if the tissue is very thick, but if the tissue is thin, it can easily recede and lose sulcus depth down to 1 or 2 mm, exposing your new margin.
Personally, if I see a patient who has at least 3 mm of sulcus depth, I evaluate the gingival levels and tooth proportion to see if I can perform a gingivectomy, reducing the sulcus depth to 1 or 1.5 mm. This reduces the risk of recession and I can follow Rule 1 above.
If the gingivectomy would result in unacceptable gingival levels, I usually plan on putting my margin below tissue half the depth of the sulcus (for a 3 mm sulcus, 1.5 mm below tissue). By doing this, if recession occurs, it will most likely stop before it exposes where the margins are placed. Of course, this risk of recession means the final gingival levels may not be ideal, but it will be more esthetic than an exposed margin on a new restoration.
VIRTUAL SEMINARS
The Campus CE Experience
– Online, Anywhere
Spear Virtual Seminars give you versatility to refine your clinical skills following the same lessons that you would at the Spear Campus in Scottsdale — but from anywhere, as a safe online alternative to large-attendance campus events. Ask an advisor how your practice can take advantage of this new CE option.

By: Frank Spear
Date: November 2, 2017
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


